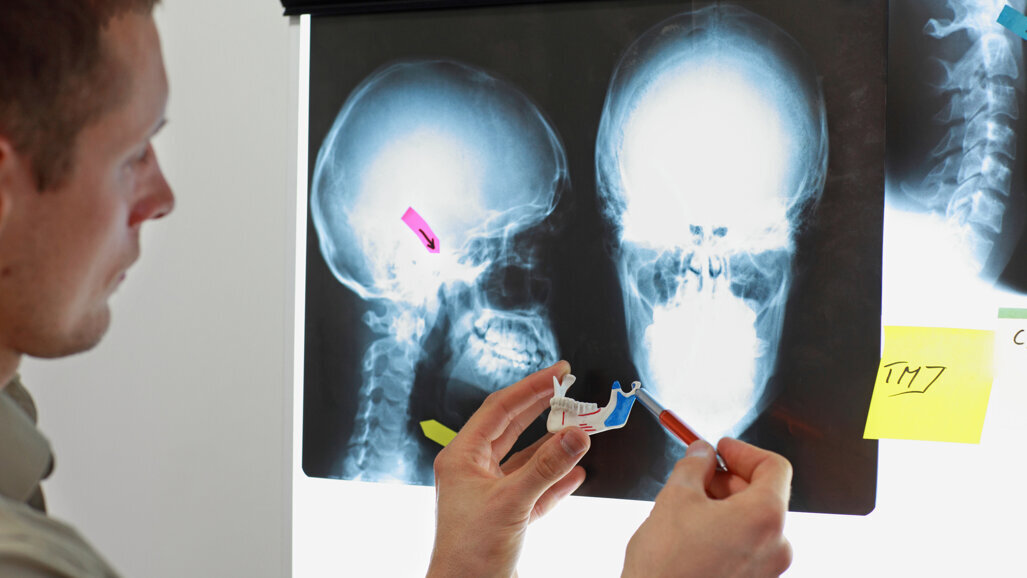
BERGEN, Norway: Existing research indicates that temporomandibular disorders (TMD) are the second most frequent source of disability and pain in the human body. A recent study evaluated the risk factors of non-resolving temporomandibular disorder in patients with long-term refractory TMD three years after their enrolment in a national interdisciplinary evaluation programme at the Haukeland University Hospital in Bergen. The study found that those patients who reported higher levels of pain intensity were more likely to later report non-resolving TMD symptoms.
At the start of enrolment, the 60 TMD patients included in the study were examined by a medical radiologist, physiotherapist, clinical psychologist, dental specialist in orofacial pain, oral and maxillofacial surgeon and pain physician. The group had suffered from TMD pain for 13.4 years on average. After meeting with the specialists, the patients were given treatment suggestions to take to their general practitioners (GPs) for follow-up.
Initially and three years later, the patients completed a questionnaire covering not just TMD symptoms and pain but also physical functioning, adverse events such as trauma, and psychosocial factors.
Though the patients overall reported satisfaction with their initial multispecialist evaluation and suggestions for treatment, three years later only 21% of the patients reported satisfaction with the follow-up provided by their GPs. After three years, 33% of the patients reported worsened TMD symptoms, 26% improved symptoms and 41% unchanged symptoms. The researchers noted that those who experienced worsening symptoms had also previously reported a much higher minimum and maximum pain intensity at baseline. This group also initially reported a higher degree of suffering as a result of pain. Statistical analysis indicated that high maximum pain intensity at baseline was a significant predictor of worsened TMD symptoms at the three-year evaluation.
As Norway is facing a shortage of TMD specialists, particularly in rural locations, general medical and dental practitioners are often dealt the task of treating TMD, even though they may lack the expertise to do so. The researchers indicated that treatment of severe TMD would ideally involve a team of specialists from both medicine and dentistry and suggested that having to resort to general doctors and dentists for follow-up may have contributed to the improvement of just ten out of the 39 patients.
The authors suggested that treatment could be improved by follow-up by the interdisciplinary team with patients and GPs and by giving patients the opportunity for responsibility for their own recovery via a rehabilitation programme with feedback. They also recommended further research on management of stress in patients with chronic pain as a factor of treatment outcome.
The study, titled “High pain intensity is a risk factor of non-resolving TMD: A three-year follow-up of a patient group in a Norwegian interdisciplinary evaluation program”, was published online on 2 May 2022 in the Journal of Pain Research.
Tags:
JÖNKÖPING, Sweden: Sweden has too few dentists in 18 of its 21 regions, and this is expected to continue until at least 2035. To close this gap, ...
MALMÖ, Sweden: Radiographic diagnostics are widely used in healthcare as they provide diagnostically important information that can help improve treatment ...
Live webinar
Tue. 24 February 2026
1:00 pm EST (New York)
Prof. Dr. Markus B. Hürzeler
Live webinar
Tue. 24 February 2026
3:00 pm EST (New York)
Prof. Dr. Marcel A. Wainwright DDS, PhD
Live webinar
Wed. 25 February 2026
11:00 am EST (New York)
Prof. Dr. Daniel Edelhoff
Live webinar
Wed. 25 February 2026
1:00 pm EST (New York)
Live webinar
Wed. 25 February 2026
8:00 pm EST (New York)
Live webinar
Tue. 3 March 2026
11:00 am EST (New York)
Dr. Omar Lugo Cirujano Maxilofacial
Live webinar
Tue. 3 March 2026
8:00 pm EST (New York)
Dr. Vasiliki Maseli DDS, MS, EdM



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East


































To post a reply please login or register