The more clinicians have learned about adhesion and composite behaviour, the more cautious they have become with layering techniques to ensure long-term success. Unfortunately, these cautious techniques—especially when aiming to reduce stress—often require significantly more chairside time. There is a growing need for a method that simplifies layering while preserving adhesive integrity and aesthetic outcomes.
Indirect restorations have proved to be highly effective in terms of adhesion, particularly because they allow the adhesive interface to mature fully before the restoration is bonded under minimal stress. This is especially true when the preparation is immediately followed by adhesive treatment—known as immediate dentine sealing. In this approach, freshly cut dentine is sealed right after tooth preparation, allowing the resin-infiltrated dentine layer, or hybrid layer, to mature in a stress-free environment during the laboratory phase of restoration fabrication. Since no shrinkage-inducing composite is placed at this stage, the adhesive layer remains undisturbed and can fully develop its mechanical properties before final bonding.
However, these indirect approaches are not always feasible in everyday clinical settings owing to time, cost or patient preference. This has led to increased interest in so-called semi-direct techniques, an approach that blends aspects of both direct and indirect workflows. The term “semi-direct” refers to restorations that are either fabricated outside the mouth on a model created from a quick impression or built directly on the tooth using a separating material such as PTFE tape. In both scenarios, the restoration undergoes extra-oral polymerisation before being returned and bonded to the tooth. This approach allows for improved control over polymerisation stress while preserving the efficiency and practicality of a chairside procedure. Although semi-direct methods offer great potential, many existing techniques are complex and demand artistic skills for free-hand anatomical shaping, limiting their accessibility in daily practice.
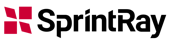
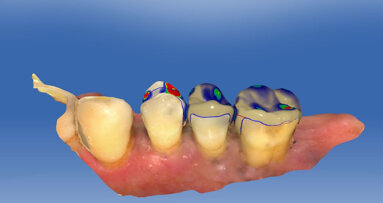
The SEAL (Stress-reduced, Esthetic, Anatomically guided, Layer-less) concept is a simplified semi-direct approach that eliminates the need for artistic modelling. Instead, it uses a preformed anatomical model, allowing clinicians to transfer morphology in a copy–paste fashion. The following case illustrates the application of the SEAL concept.
Technique description
Treatment focused on a mandibular first molar with existing Class I and V composite restorations (Fig. 1). The tooth was asymptomatic, and cold testing revealed a normal response. A distal carious lesion, which was not clinically visible, was first suspected during routine screening and its extent clearly identified on the panoramic radiograph (Fig. 2).
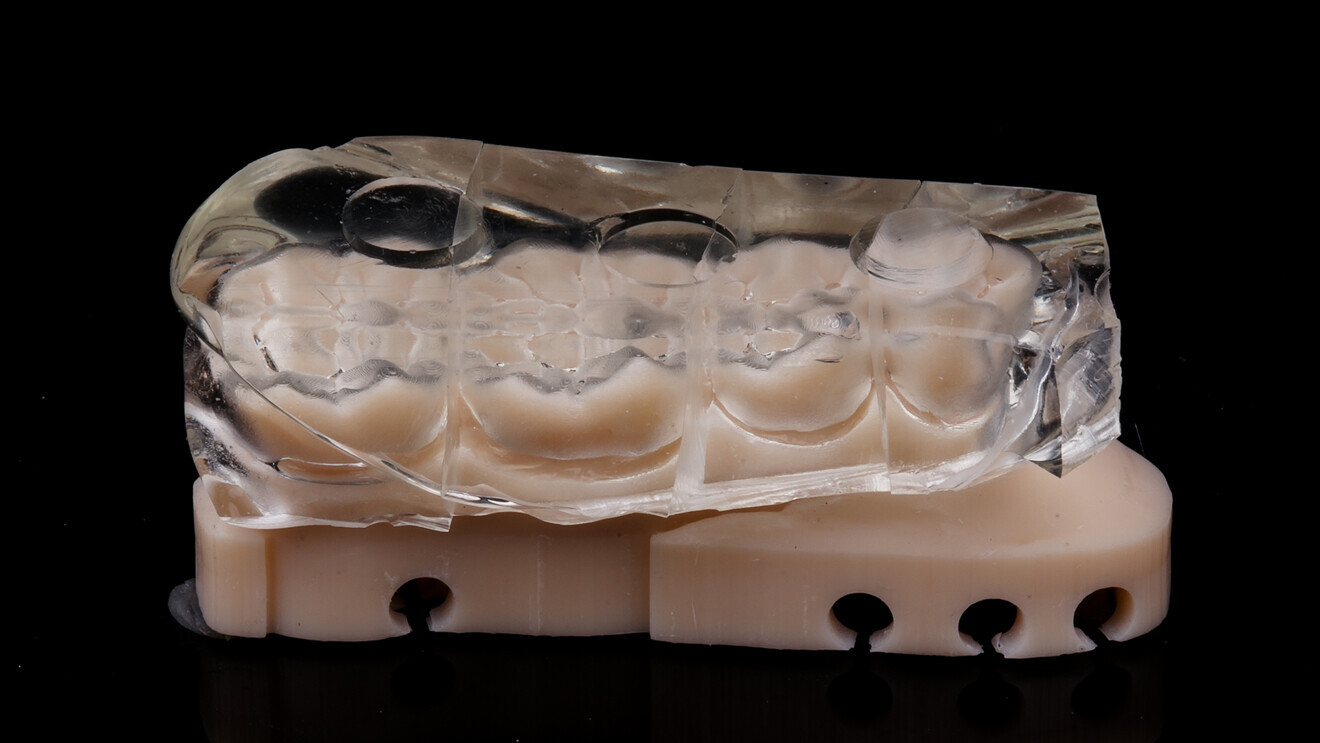
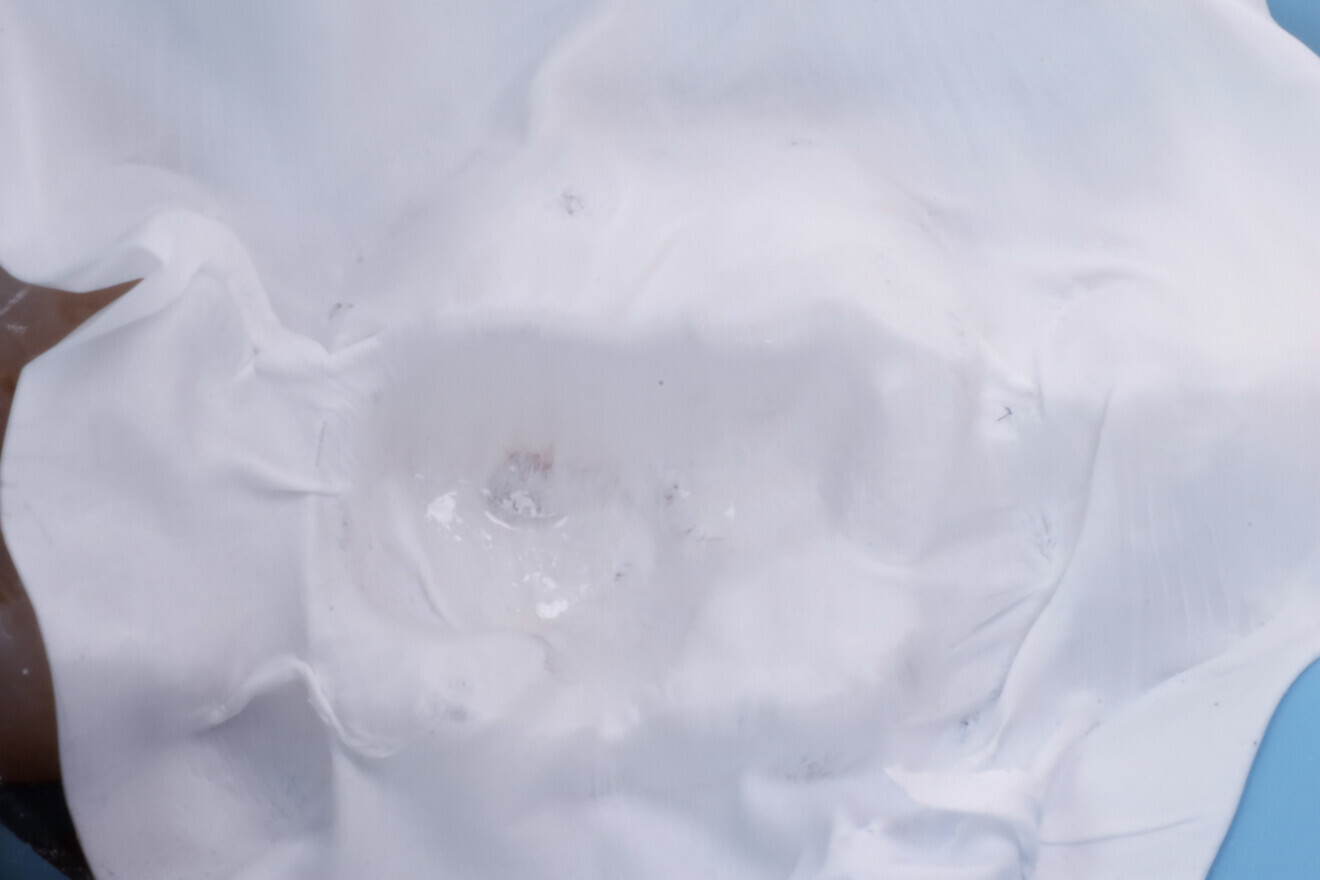
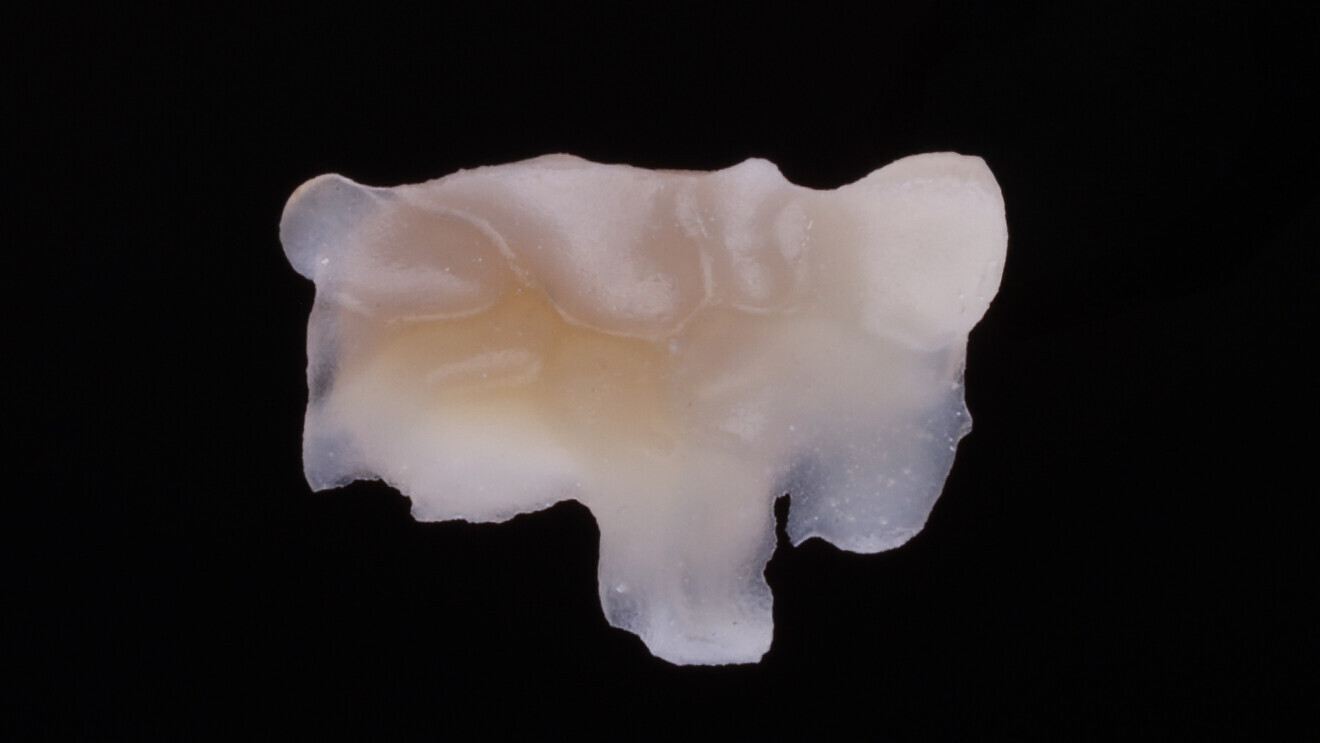
After isolation using a dental dam (Isodam, 4D Rubber; Fig. 3), the old restorations were removed, revealing the distal carious lesion (Fig. 4). Caries detection dye (CARIES DETECTOR, Kuraray Noritake Dental) was applied for visual confirmation (Fig. 5).



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East


























































To post a reply please login or register