Case summary
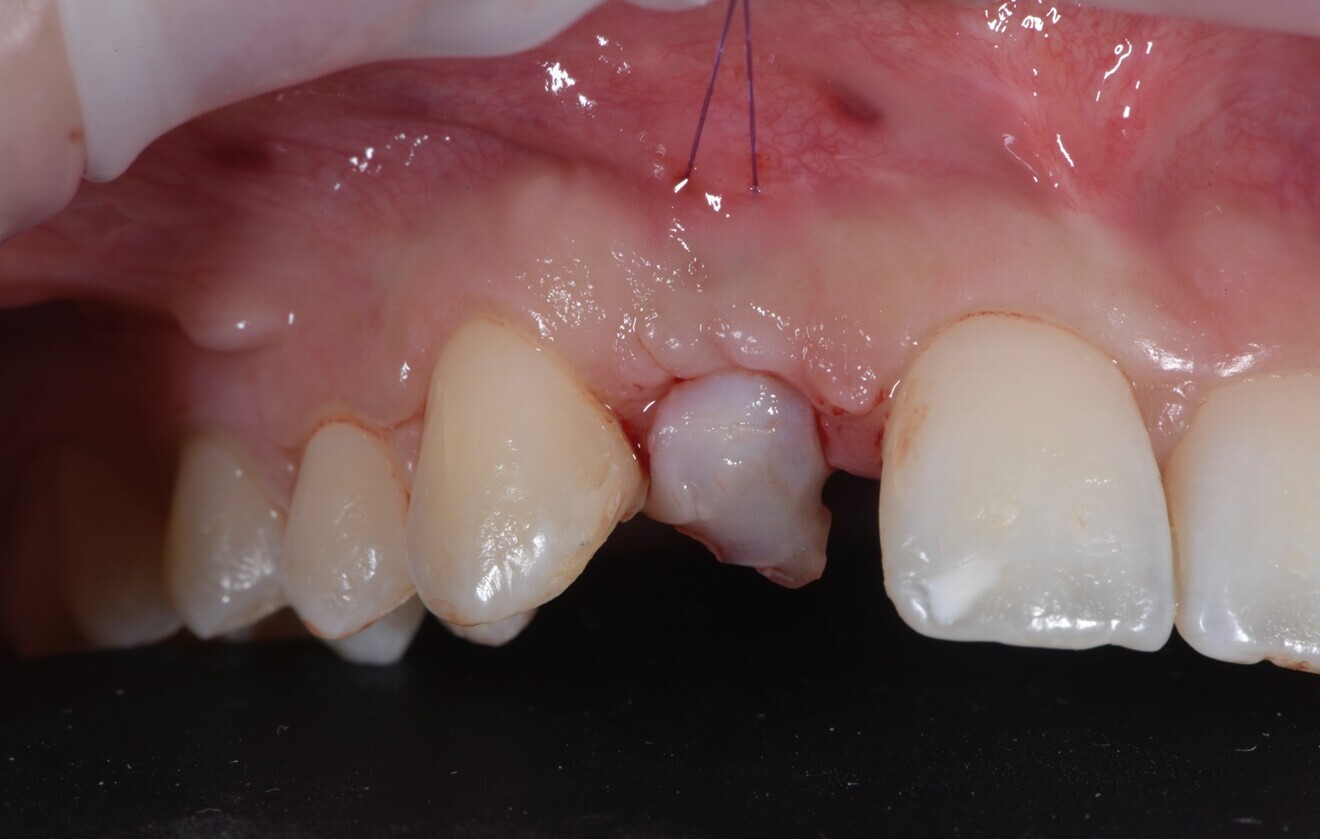
A 26-year-old partially edentulous female patient was referred to our clinic with an aesthetic concern in the region of the maxillary right lateral incisor. Clinical examination revealed an osseointegrated but malpositioned implant. The peri-implant soft tissue appeared thin and inflamed. Additionally, a dark-greyish discoloration was visible through the gingiva—referred to as the umbrella effect—caused by the loss of peri-implant bone and show-through of the titanium implant (Fig. 1).
Periapical radiographs showed bone contact on the mesial and distal aspects of the implant. However, clinical probing and CBCT revealed labial and palatal bone loss, consistent with a labially malpositioned implant (Fig. 2).
The patient reported congenital agenesis of the maxillary right lateral incisor and placement of the implant several years prior. After a comprehensive discussion of the treatment options, the patient consented to implant removal and future replacement after bone regeneration. This decision was based on aesthetic concerns and the high risk of further bone loss during medium- to long-term follow-up. The patient was healthy and a non-smoker.
At the initial visit, digital impressions were obtained using the Medit i700 scanner. Periapical radiographs and standardised intra-oral and extra-oral photographs were also acquired. A virtual diagnostic wax-up was generated to guide treatment planning. On the day of surgery, local anaesthesia was administered, and the implant was atraumatically removed using the reverse torque explantation technique. The surgical site was debrided and cleaned, and Type I collagen was applied to the socket (Fig. 3).
A provisional Maryland bridge was bonded to restore the edentulous area aesthetically. After an eight-week healing period, a vertical GBR procedure was performed by two experienced clinicians (MT and SMM). Antibiotic prophylaxis was administered (amoxicillin 2 g 1 hour preoperatively, followed by 1 g twice daily for eight days). The patient also rinsed with 0.2% chlorhexidine for 1 minute before surgery, and the surgical site was isolated with a sterile drape.
Anaesthesia was delivered using 4% articaine with 1:100,000 adrenaline (Ubistesin, 3M ESPE). A crestal incision through the keratinised mucosa was made using a No.15c blade, and a full-thickness flap was elevated. Vertical releasing incisions were placed two teeth away, both mesially and distally (Fig. 4).
The recipient site was debrided, and autogenous cortical bone was harvested from the ipsilateral mandibular ramus (external oblique ridge) using a bone scraper (MICROSS, META). A resorbable collagen membrane (OssMem Hard, Osstem Implant) was secured on the palatal aspect of the defect. A one-to-one mixture of autogenous bone and anorganic bovine bone (A-Oss; particle size: 0.25–1.00 mm; 0.5 g in total; Osstem Implant) was packed into the defect. The membrane was then stabilised with two additional fixation screws.
After eight months of uneventful healing, a CBCT scan (6 × 8 cm field of view, 90 kVp, ~ 7 mA) was performed. A prosthetically guided surgical guide was designed to ensure optimal implant positioning. Under local anaesthesia, a flap without vertical releasing incisions was raised. A new implant (TSIII SOI, 3.5 × 11.5 mm; Osstem Implant) was placed using a fully guided protocol (Fig. 5). After implant placement, a connective tissue graft was harvested from the palatal area (first premolar to first molar region) and sutured to thicken the peri-implant mucosa (Fig. 6). The patient was provided with detailed postoperative care instructions and medication.
After four months of healing, a minimally invasive uncovering procedure was performed, and a digital impression was taken. Two weeks later, a screw-retained provisional restoration was delivered to contour the peri-implant soft tissue (Figs. 7 & 8).
After approximately three months, a final impression was captured, and a definitive porcelain-veneered zirconia crown was fabricated and cemented over a titanium hybrid abutment (Fig. 9). The occlusion was carefully adjusted, and the patient was enrolled in a structured maintenance programme with four-month recall intervals. At the one-year follow-up, the implant demonstrated excellent clinical and radiographic outcomes, showing stable soft tissue and no signs of inflammation or bone loss. The patient reported full satisfaction with the aesthetic and functional results.


 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East













































To post a reply please login or register