Ceramic printing is another exciting area. Emerging systems now allow for printing lithium disilicate restorations—an impressive step forwards, even if the technology isn’t widely accessible yet.
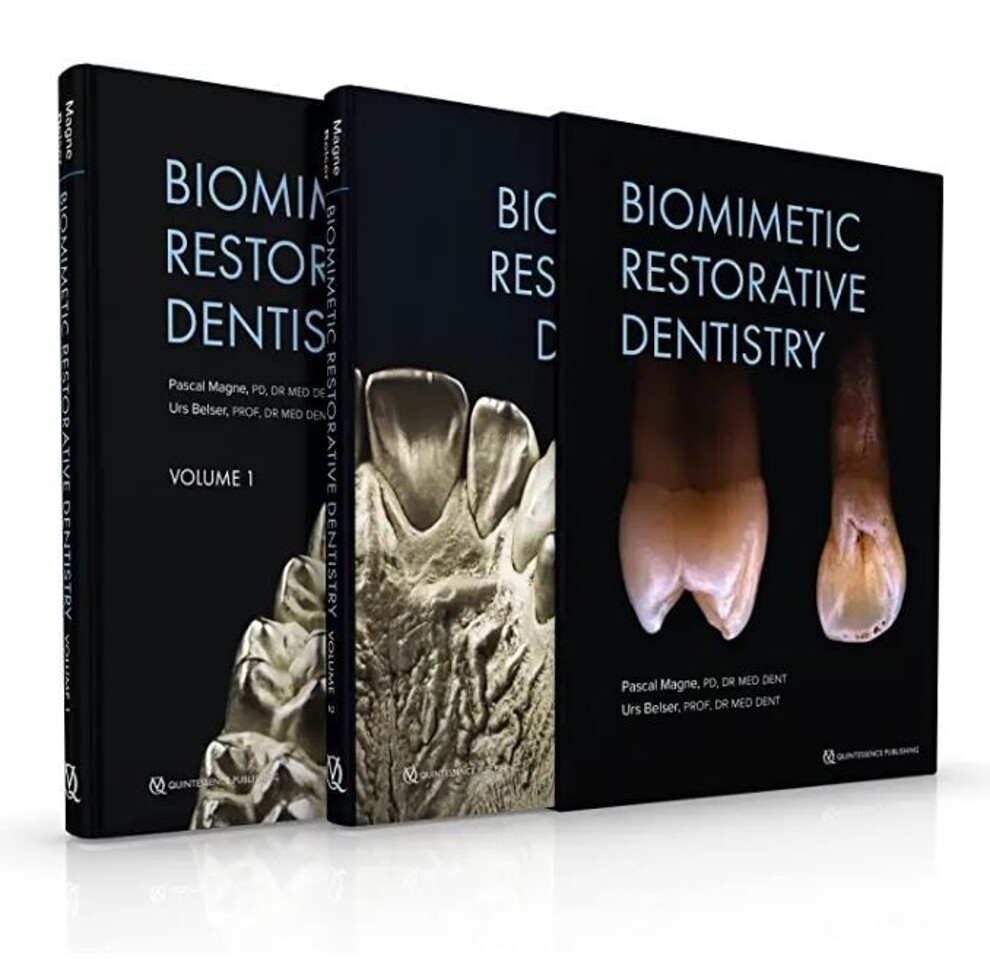
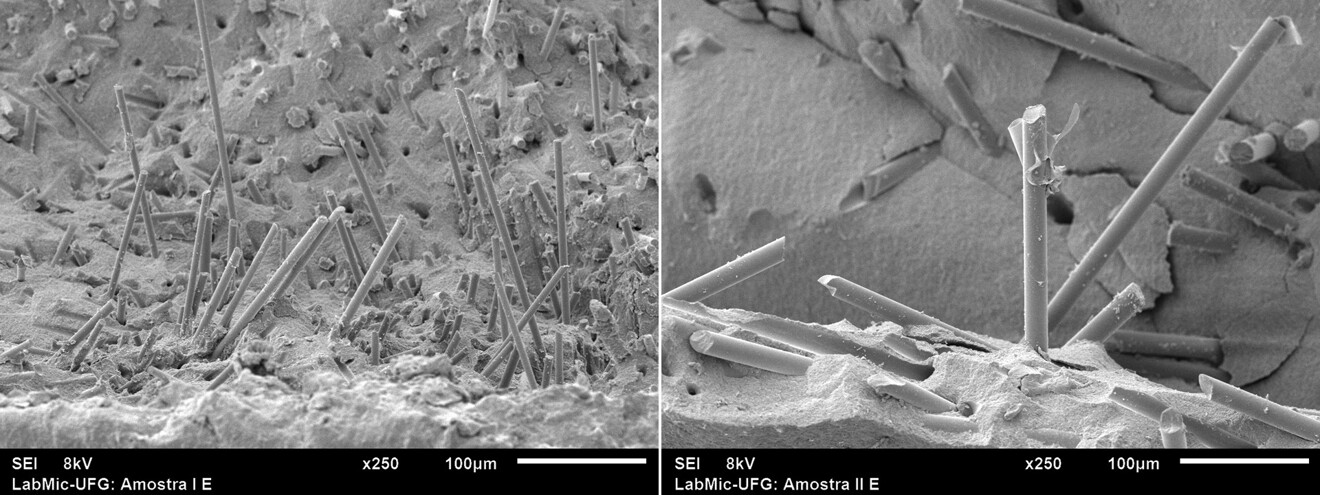
I’m very interested in new developments in FRCs in general. Research from Finland on hybrid FRCs—combining large and small fibres—has showed great promise.12 Imagine printable FRCs, CAD/CAM blocks or even fibre-reinforced cements. That’s the kind of innovation that I believe will shape the next decade in restorative dentistry.
If you could redesign dental education from scratch, what would you prioritise to prepare students for the future of biomimetic dentistry?
To me, biomimetic restorative dentistry is a fully integrated discipline—and I believe that it should be introduced from day one in dental school. This early exposure is crucial. Take morphology, for example: many students struggle to see its relevance, but when you frame it through the lens of biomimetics, where shape equals function, mechanics and aesthetics, it suddenly makes sense. Biomimetic dentistry is about preserving biology—keeping the pulp alive—then restoring function and finally aesthetics as the cherry on top.
Leaving academia was a big decision for me. I’ve always seen myself as an educator at heart. I eventually left to build something I had dreamed of for years: an ideal learning environment. That’s how Magne Education was born here in Beverly Hills, supported by the partnership and vision of master dental technician Sam Alawie, owner of Beverly Hills Dental Laboratory.
We offer a wide range of programmes in English and Spanish—from online learning through our PRESSroom lecture series to one-on-one distance mentoring through our mentoring programme, where clinicians bring their cases and we work through treatment planning together. We also run an in-person mini-residency called the Continuum—five courses over 15 days—and a more intensive one-week bootcamp for those who can’t travel multiple times. It’s a deep dive into morphology, aesthetics, direct composites, CAD/CAM and more. For me, this is a dream realised: creating a space where we teach dentistry the way it should be taught—starting with the tooth, not the restoration.
What advice would you give to young dentists who want to follow in your footsteps?
To young dentists, be mindful of misinformation, especially on social media. Many still misuse terms like “biomimetic” or confuse old and new concepts. Remember that a concept that teaches you to remove more tooth structure than a classic crown preparation cannot be called biomimetic. Even research can be misleading—clinical data is valuable, but in vitro studies are underrated and often offer deeper insights. You need to get the full picture: always read the whole article, not just the abstract, and evaluate it with a critical mindset.
But most importantly, follow your passion. Find the area of dentistry that excites you and stay focused on it—distraction is the biggest challenge today. Also, don’t do it alone: find a mentor. A good mentor will guide, protect and inspire you. I’ve been blessed with several mentors, and I wouldn’t be where I am without them, Drs Belser, Douglas and Didier Dietschi, and my brother.
I want to finish on a more personal note and give all glory to my ultimate mentor, who taught me humility, forgiveness, compassion and faith while always providing practical and spiritual instructions. He is “the light of the world” (John 8:12).



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East













































To post a reply please login or register