Discussion
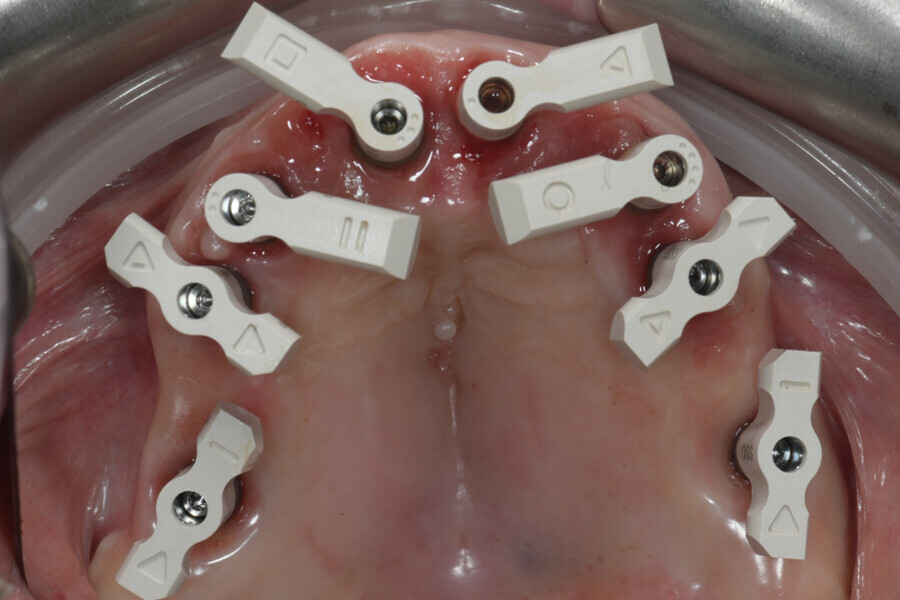
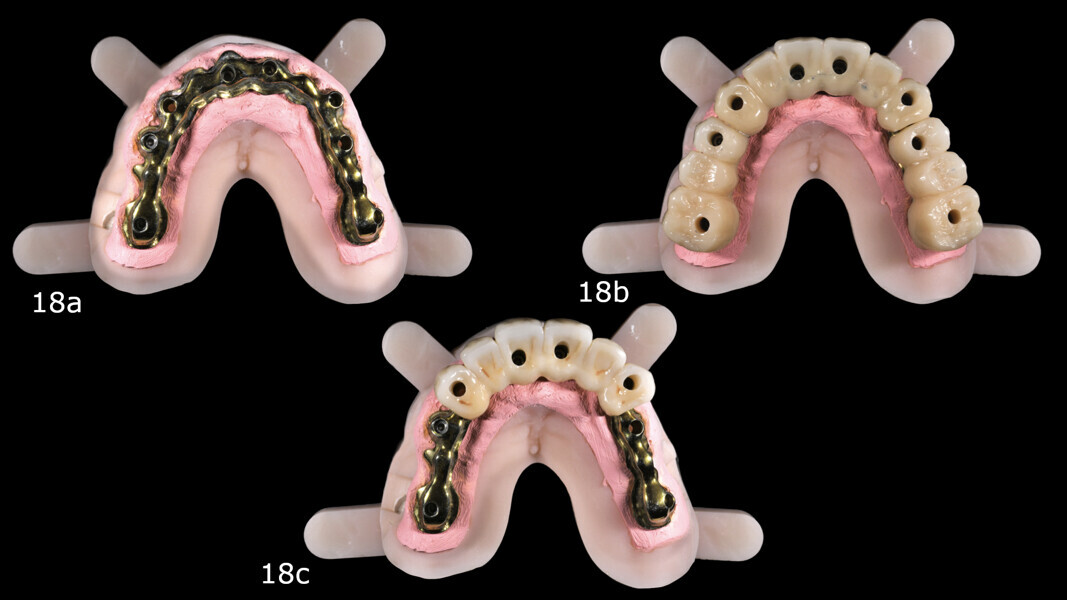
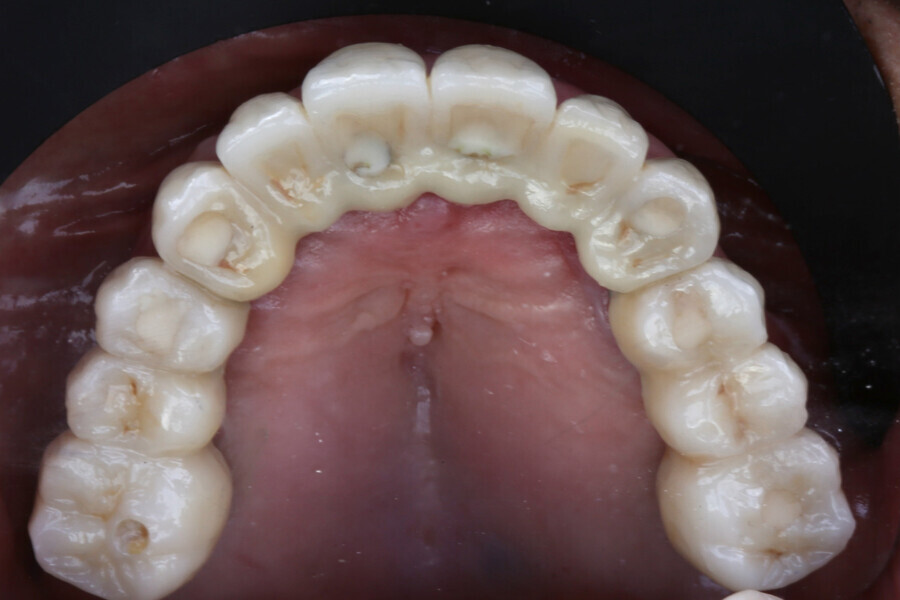
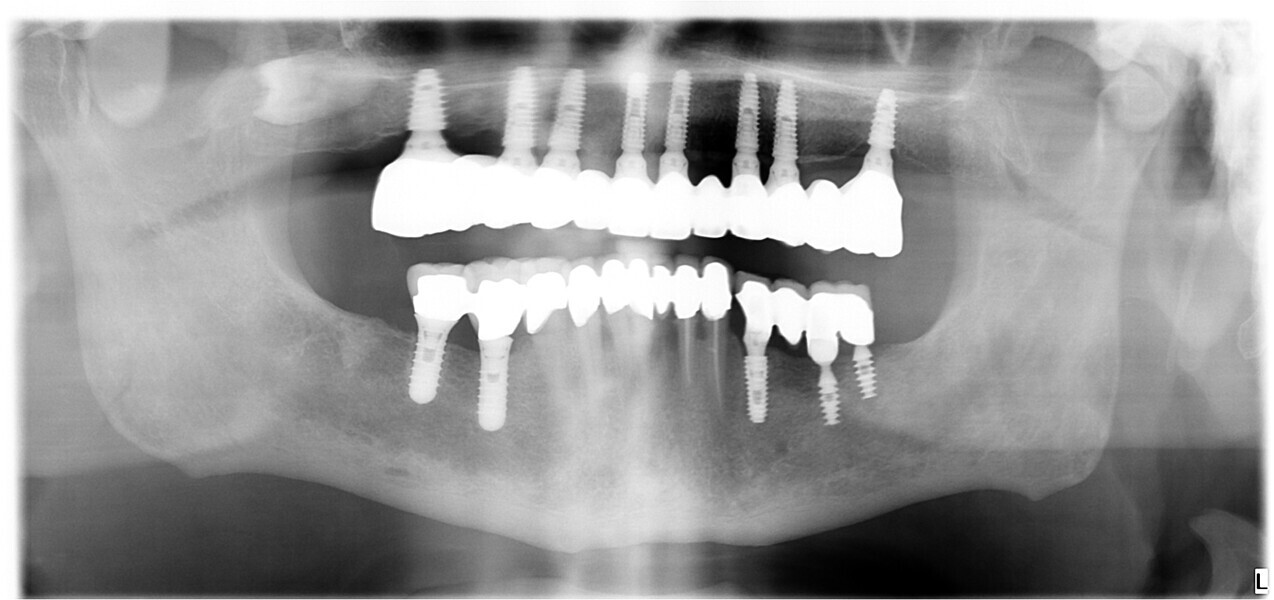
This case highlights the evolving role of digital technologies in achieving high precision and predictability in full-arch implant rehabilitation. One of the key determinants of long-term success in such rehabilitation is the passive fit of the definitive prosthesis. A truly passive fit minimises mechanical stress on the implants and surrounding bone, reducing the risk of biological or technical complications such as peri-implantitis, screw loosening or framework fracture.15, 16 In this case, a combination of multi-unit abutments, intra-oral scanning and a CAD/CAM metal framework contributed to verifying passive fit using the one-screw test and tactile evaluation.15
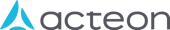
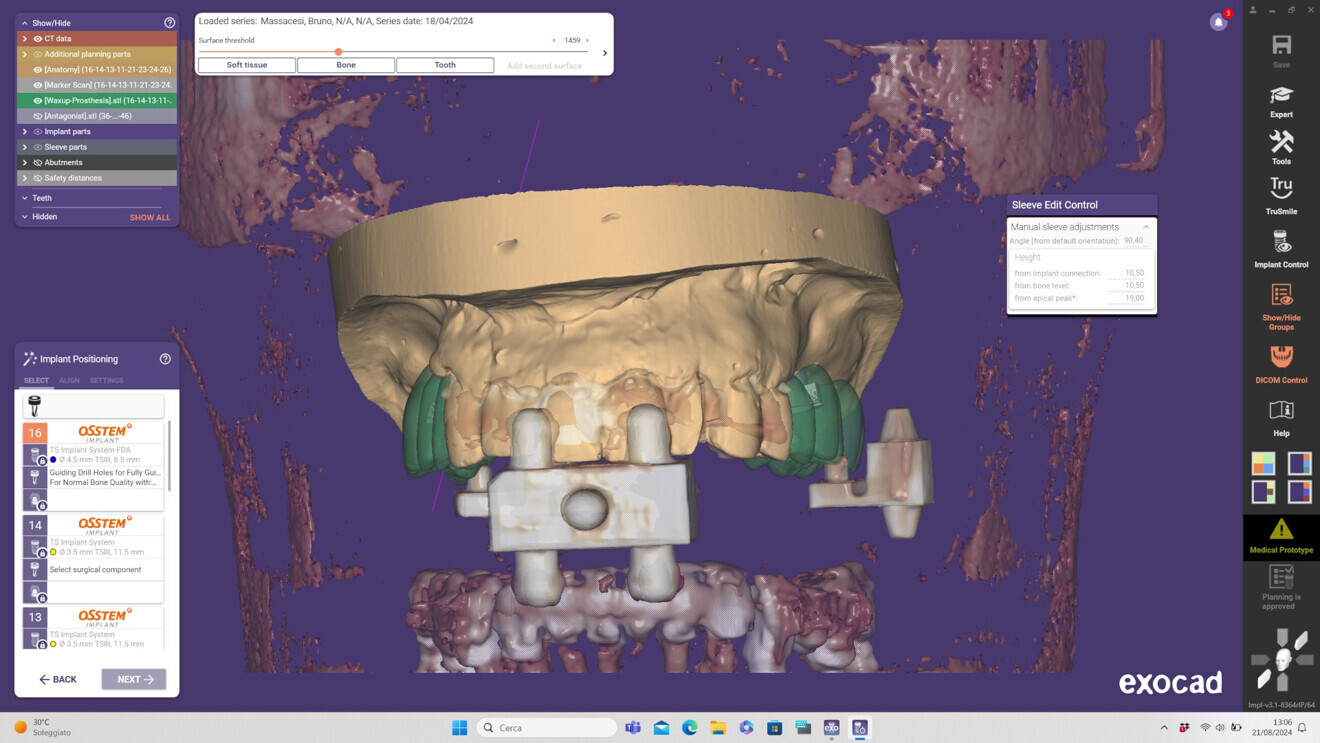
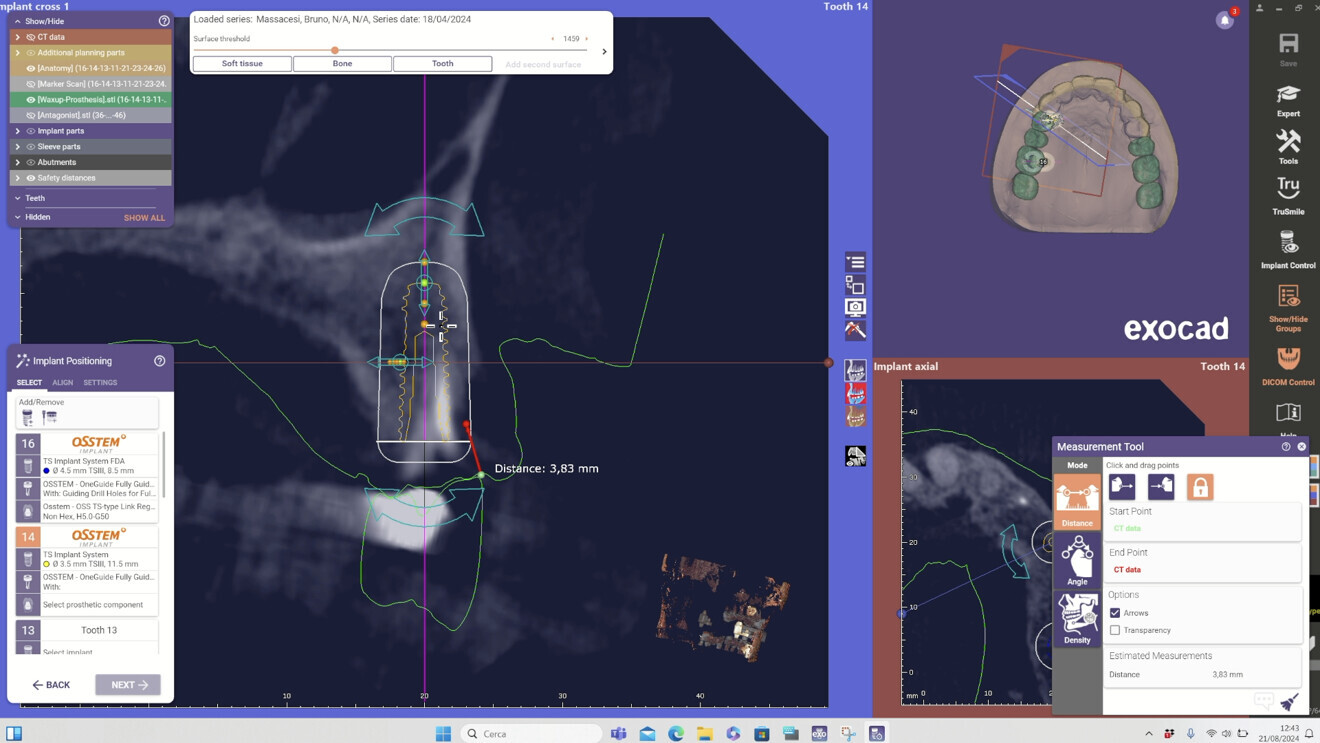
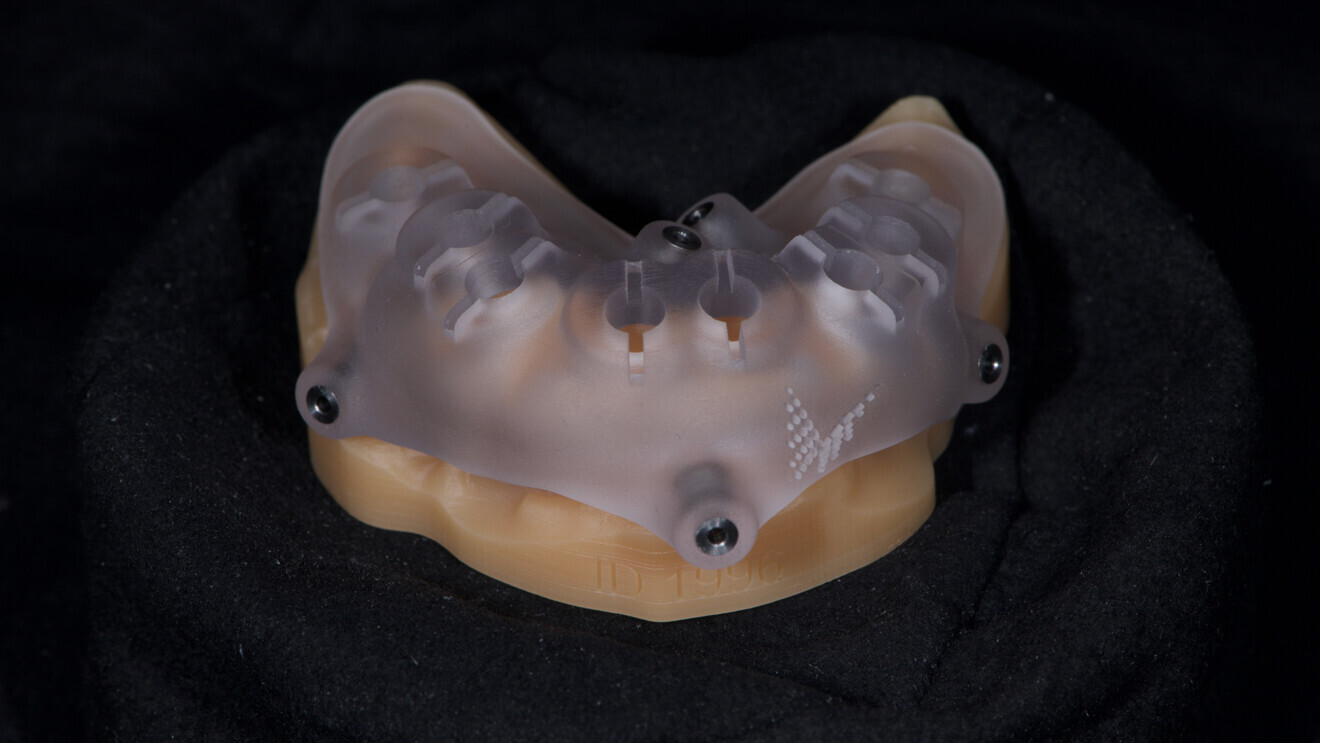
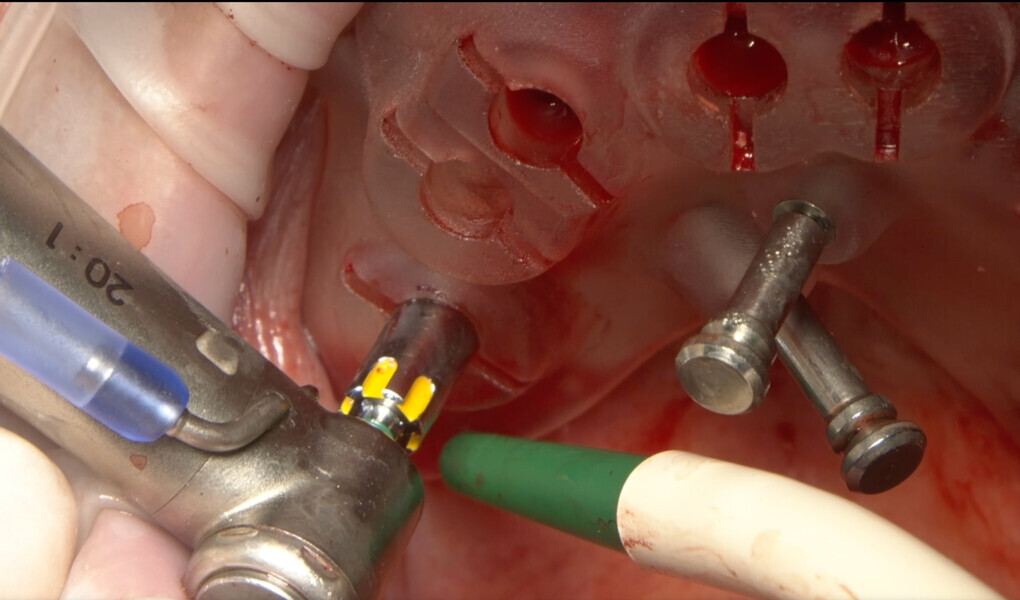
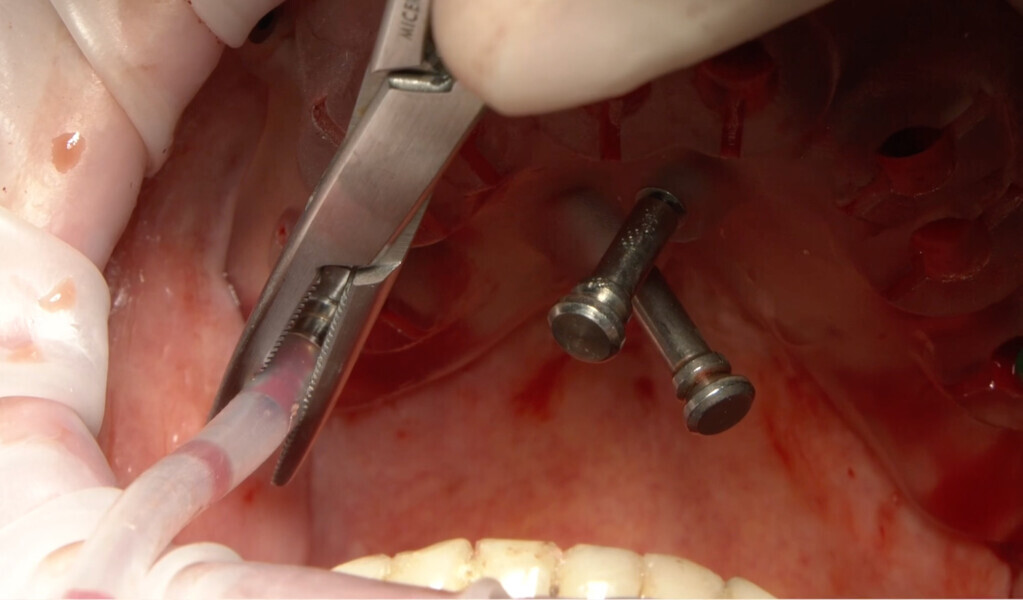
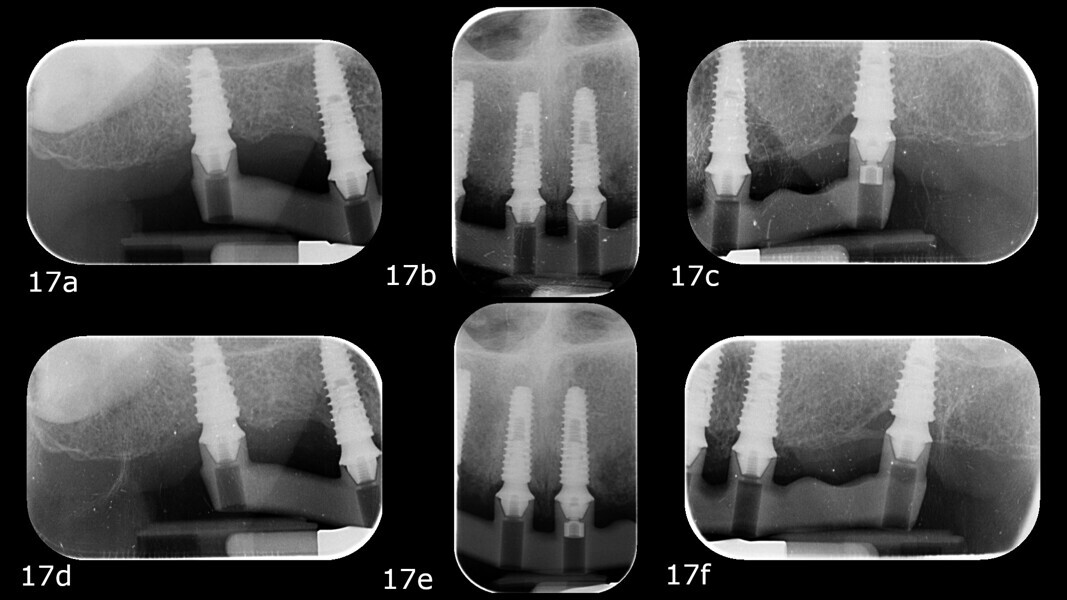
Another critical factor that influences long-term clinical outcomes is the 3D positioning of implants. Accurate implant placement in terms of depth, angulation and mesiodistal spacing directly affects prosthetic fit, occlusal harmony and load distribution.17 In the edentulous maxilla—where anatomical constraints and soft-tissue mobility challenge manual techniques—the use of computer-guided surgery proves especially valuable. In this case, fully guided implant placement was facilitated by digital planning and a 3D-printed surgical guide anchored by pins.18 This protocol enabled a minimally invasive approach and the execution of a crestal sinus lift, illustrating how guided surgery can manage anatomical complexity with minimal invasiveness. The precision afforded by virtual planning translates directly into surgical accuracy, improving both prosthetic predictability and patient outcomes.19
The integration of intra-oral scanning technologies and CBCT imaging allowed for a seamless, non-invasive digital workflow from diagnostic evaluation to prosthesis delivery. This approach enabled precise implant planning, prosthetic design and the fabrication of a customised surgical guide, all aligned with the patient’s anatomy and prosthetic requirements. In contrast to traditional workflows, digital tools reduce the margin for manual error and offer significant advantages in terms of patient comfort, efficiency and reproducibility.20
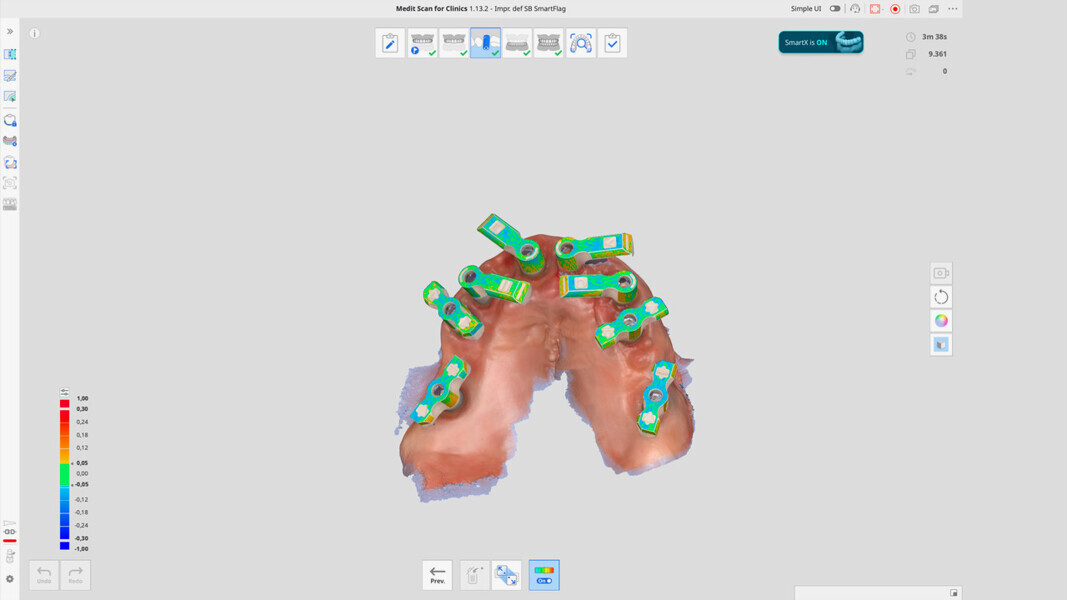
A key innovation in this case was the use of Medit SmartX, an AI-driven platform that enhances the accuracy of intra-oral scanning by optimising scan body recognition and alignment. The system leverages AI to reduce potential mismatches during full-arch data acquisition—one of the most critical phases in digital implantology. Medit SmartX provided a streamlined scan protocol, combining straight and zigzag patterns in the anterior regions and straight scans in the posterior regions, ultimately resulting in higher-quality datasets and better prosthetic fit. These improvements were especially beneficial in managing a fully edentulous maxilla, where the lack of anatomical landmarks can compromise data integrity. The Medit SmartX workflow may optimise scan data alignment principles and scanning settings to achieve more precise data compared with conventional processes. This would help better highlight the technical advantages of Medit SmartX.
The integration of precise and predictable surgical kits, such as those used in this clinical case report, combined with implants engineered with advanced surface technologies designed to enhance osseointegration—Osstem Implant’s SOI surface—plays a vital role in achieving reliable and consistent clinical outcomes. These innovations not only streamline surgical procedures, but also support long-term success in implant dentistry, making them indispensable tools for modern dental practitioners.
Despite the successful outcome, this case report presents certain limitations. As a single case, the results cannot be generalised across all clinical scenarios. The patient had favourable bone volume and good systemic health, conditions that may not be present in more compromised individuals. Additionally, while the Medit SmartX system showed promising results, its long-term performance, reproducibility across different operators and integration with other software ecosystems warrant further investigation. The assessment of passive fit relied on clinical methods that, although widely accepted, remain partially subjective without verification via digital stress analysis or industrial-level measurements. Moreover, the time and effort required to learn to effectively employ AI-assisted tools and fully digital workflows remains significant. Successful application requires not only access to advanced equipment but also a deep understanding of digital planning, software logic and potential intra-operative adjustments.
Conclusion
This case underscores the clinical value of fully digital workflows supported by AI-assisted technologies in achieving accurate, efficient and patient-centred full-arch rehabilitation. The combination of guided surgery, precise 3D implant positioning and digital verification protocols enables clinicians to deliver prostheses with high functional and aesthetic predictability. While the integration of systems like Medit SmartX can enhance scan fidelity and prosthetic fit, further studies—including clinical trials and multi-operator analyses—are needed to fully validate these innovations and determine their broader applicability.



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East


















































To post a reply please login or register