Laser is becoming essential for every modern dental practice. Moreover, from an educational standpoint, there are many benefits in terms of the personal and professional development of the practitioner. In this interview, Dr Michał Nawrocki explains how laser dentistry has helped to advance his practice and career and why dental laser, and Fotona’s LightWalker in particular, has become an essential part of his daily practice.
Dr Nawrocki, you have been using laser technology since 2016. Looking back at your journey as a laser dentist, how has LightWalker impacted your everyday practice?
I started my great adventure with Fotona’s LightWalker in 2016. Before that I had used a diode laser, but it was insufficient for me, and to be honest my knowledge of lasers, physics, indications and procedures was incomplete at the time. Then in January 2016, I invited Dr Ilay Maden to my clinic to conduct a course and teach my colleagues and me about various Er:YAG and Nd:YAG procedures with the LightWalker laser. A few months later, I decided to extend my knowledge about lasers by attending the Master of Science in Lasers in Dentistry presented by Prof. Norbert Gutknecht in Aachen. Now, I cannot imagine continuing my daily practice and treatments without having LightWalker. Sometimes, I use it as an additional tool during certain procedures, but very often it’s a crucial and necessary tool for me to use to conduct a particular procedure.
What procedures do you perform with laser?
Laser can be used in all fields of dentistry; however, I am mainly focused on implantology and surgery, as well as prosthodontics. In prosthodontics, it can be used for sulcus conditioning, preparation for veneers and removal of complete ceramic crowns, as well as during more challenging procedures like crown lengthening before tooth preparation. We can use it in gingivectomy (Nd:YAG laser) and bone recontouring (Er:YAG laser).
All my surgery cases are finished with photo-biomodulation using the Nd:YAG Genova handpiece. I have observed that wound healing is much faster and better in such cases owing to pain reduction, disinfection, reduction of oedema and the laser’s analgesic function. Sometimes, I have to conduct an endodontic treatment during the procedure (which is quite rare and normally done by my colleagues), in which case I really appreciate the deep disinfection with Nd:YAG, which offers the highest bacterial reduction in comparison with other wavelengths, and the Er:YAG SWEEPS [shock wave-enhanced emission photoacoustic streaming] procedure, which provides the most effective cleaning and disinfection. With surgical treatments, I use both wavelengths in almost all cases. Even when performing an easy and fast tooth extraction, I can use Er:YAG for granulation tissue removal, followed by Nd:YAG for disinfection, clot stabilisation and finally photo-biomodulation. Of course, I use laser before implant insertion, as well as when complications appear.
In your opinion, what are the main benefits of choosing a laser system that includes two complementary wavelengths, such as Er:YAG and Nd:YAG, especially in the field of oral surgery?
Very often, we combine these two wavelengths to conduct treatment in a fast, safe and predictable way. For me, it’s crucial to use these two complementary wavelengths—the interaction between the tissue and laser beam is quite different, and owing to these differences in absorption, transmission and scattering, we obtain different actions. For example, during root apicectomy, after flap elevation, I remove granulation soft tissue with the Er:YAG laser using the H14 handpiece with a cylindrical tip (or when I want to be more precise—a Varian tip) and the apicectomy is done with the H02 non-contact handpiece. As the next step, I conduct deep disinfection with the Nd:YAG laser (transmission in hydroxyapatite and absorption in pigmented bacteria) before bone augmentation. Finally, I finish the treatment with photo-biomodulation using the Nd:YAG laser. As you can see from this example, I need both of these two complementary wavelengths to achieve final success with fast healing and proper bone regeneration.
“We can use LightWalker for all implantology cases”
One of your main fields of specialisation is implantology. Where does the laser fit in this field?
We can use LightWalker for all implantology cases. Sometimes, it’s only needed for better and faster wound healing (photo-biomodulation with the Nd:YAG laser), but very often it is necessary to conduct the treatment. For me, it’s the most important device during immediate implantation with immediate loading, especially when the bone must be very precisely cleaned of granulation soft tissue and disinfected. In the meantime, we can also provoke bleeding of the bone using the Er:YAG laser for superficial bone ablation. I also really appreciate the use of laser during bone grafting with the Khoury method. Sometimes, I combine this technique with immediate implantation, especially in the aesthetic zone. Then, after bone shield fixation, I can use the laser for bone recontouring. With the Er:YAG laser, it’s done very precisely—I remove sharp edges and create an emergence profile for the crown—and most importantly, everything is safe for the shield (almost no vibration, so we don’t lose stability) and the implant (no thermal effect).
Of course, we can also use the Er:YAG laser for more common and “easy” procedures—like implant uncovering (Er:YAG). The healing is faster and we avoid suturing, but of course, even with the thin chisel tip, some amount of soft tissue is vapourised—so it cannot be conducted in all cases.
In 2018, you defended your master’s thesis at RWTH Aachen University titled Comparison of Two Methods of Periimplantitis Treatment with the Use of Nd:YAG and Er:YAG Laser. Can you tell us more about that research?
Owing to the increasing number of implants being placed, the development of peri-implantitis is a growing concern and one of the primary challenges in present-day dentistry. In cases of inflammation, it is necessary to implement treatment, or risk implant loss. However, until now, no uniform protocol or procedure has been defined which could be considered the best and the most effective solution. Different methods of treatment of tissue inflammation around the implant are used, depending on the extent of inflammation, method availability, type of defect, and skills and experience of the dental surgeon.
We know that laser can be used for the treatment of inflammation in soft and hard tissue around implants, such as mucositis and peri-implantitis. I wanted to investigate what kind of procedure would be the most effective and minimally invasive—so the question was whether we could use a minimally invasive, flapless procedure for proper treatment and solve the problem of inflammation.
The procedures were conducted with Er:YAG and Nd:YAG lasers. In the first group of patients, a mucoperiosteal flap was elevated in order to gain better access to the operative area, while the second group of patients was treated using a more minimally invasive procedure without the flap method. The assessment of treatment effectiveness involved clinical and radiographic examination before the surgical procedures and three months after the laser procedures. After conducting the intra-oral examination and defining plaque, probing depth and bleeding on probing indices, photographic documentation of a given area was performed, bitewing and occlusal surface radiographs were taken, and professional scaling and root planing were subsequently carried out.
Based on my research, we know that non-surgical treatment of peri-implantitis is effective and very often reduces inflammation. Of course, when we have severe defects, it’s impossible to avoid a surgical procedure to elevate a flap to get proper access to the defect. In such cases too, we should use a non-surgical procedure as a first step to decrease the inflammation and, after two to three weeks, perform the flap procedure.
Can you describe your standard laser protocol for peri-implantitis treatment?
Firstly, we have to distinguish mucositis from peri-implantitis with a radiovisiograph and with the use of a periodontal probe. If possible, I remove the prosthetic restoration to get better access for the treatment. In our surgical protocol, we have five steps: (1) removal of granulation tissue with the use of the Er:YAG laser (cylindrical tip); (2) decontamination of the implant surface with Er:YAG; (3) surface ablation of infected bone with Er:YAG; (4) reduction of bacteria in the bone with the Nd:YAG laser; and (5) photo-biomodulation with the Nd:YAG laser (after flap closure).
In our non-surgical procedure, there are only four steps—I skip deep disinfection with the Nd:YAG laser owing to the 1,064 nm wavelength’s high absorption in titanium (it’s not possible without elevating a flap to disinfect only the bone and not harm the implant surface). As I mentioned, the flapless procedure is most often my first option, and when the defect is severe, I decide on a surgical procedure as the second stage.
After the procedure, the same restoration is generally placed in the mouth (after corrections if necessary). Sometimes, depending on the type of bone defect, I decide to conduct bone regeneration with the use of bone substitute and collagen membranes. In such cases, I have to remove the restoration and, after peri-implantitis treatment with the use of laser and bone augmentation, close the flap with cover screws, leaving the patient with no restoration (posteriorly), not even a temporary one, for two to three months.
“[...] peri-implantitis is a huge challenge nowadays; statistically, in 20% of cases peri-implantitis develops and in 40% of cases mucositis develops around inserted implant”
What are the benefits of LightWalker for the treatment of peri-implantitis in your everyday practice?
As I mentioned, the treatment of peri-implantitis is a huge challenge nowadays; statistically, in 20% of cases peri-implantitis develops and in 40% of cases mucositis develops around inserted implants. Treatment with the use of Er:YAG and Nd:YAG lasers is very effective, fast and comfortable for both patients and practitioners. We can use a minimally invasive, non-surgical treatment, which very often is highly effective, and thus avoid a surgical procedure. However, it’s very important that we use our lasers with proper parameters to protect the soft and hard tissue and not alter the implant surface. We can thoroughly remove bacterial biofilm from the implant surface without altering it, and we have the possibility of re-osseointegration. Of course, we have to be aware of risk factors and aim to avoid them, understand what the reason for the disease was and solve the underlying problem. Sometimes, it’s only improper oral hygiene, while other times, we must change or correct the restoration. Each case is individually treated.
Could you share with us some of your more challenging cases of peri-implantitis and explain how the treatment was performed?
Case 1 was a patient who presented with deep pockets (9 mm), bleeding on probing and visible purulent effusion (Figs. 1–7) and was treated with a non-surgical protocol.
Fig. 1: Initial situation.
Fig. 2: Pocket depth measurements.
Fig. 3: Bleeding on probing.
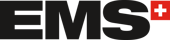
Figs. 4 & 5: Use of the Er:YAG laser Varian tip for granulation tissue removal, implant surface decontamination...
...and surface ablation of infected bone.
Fig. 6: Photo-biomodulation with the Nd:YAG laser.
Fig. 7: Final results after three months. No sign of inflammation.
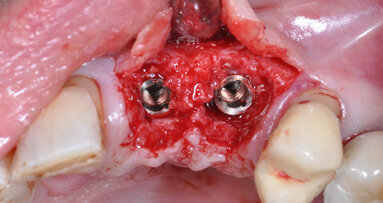
In Case 2, the patient preferred a surgical procedure with bone augmentation, as a consequence of bone graft complication and graft exposure (Figs. 8–12).
Fig. 8: Initial situation.
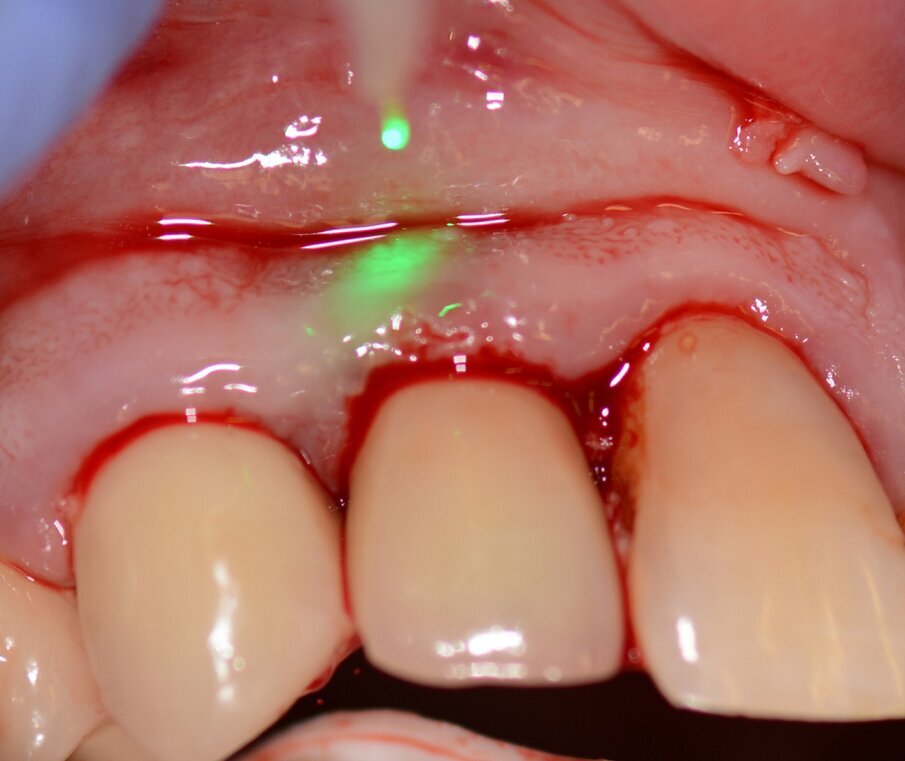
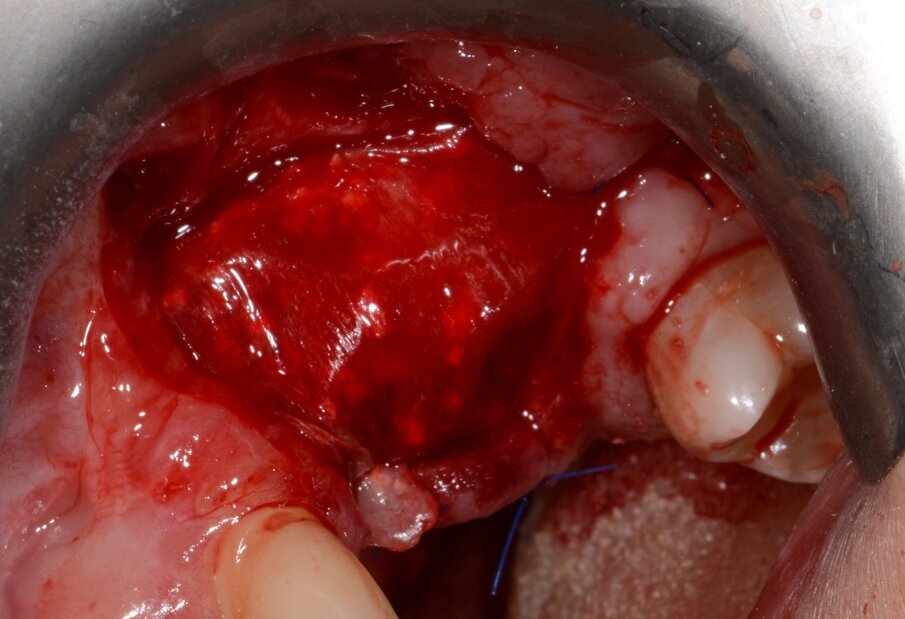
Fig. 9: Granulation tissue visible after flap elevation.
Fig. 10: Granulation tissue removal with Er:YAG laser.
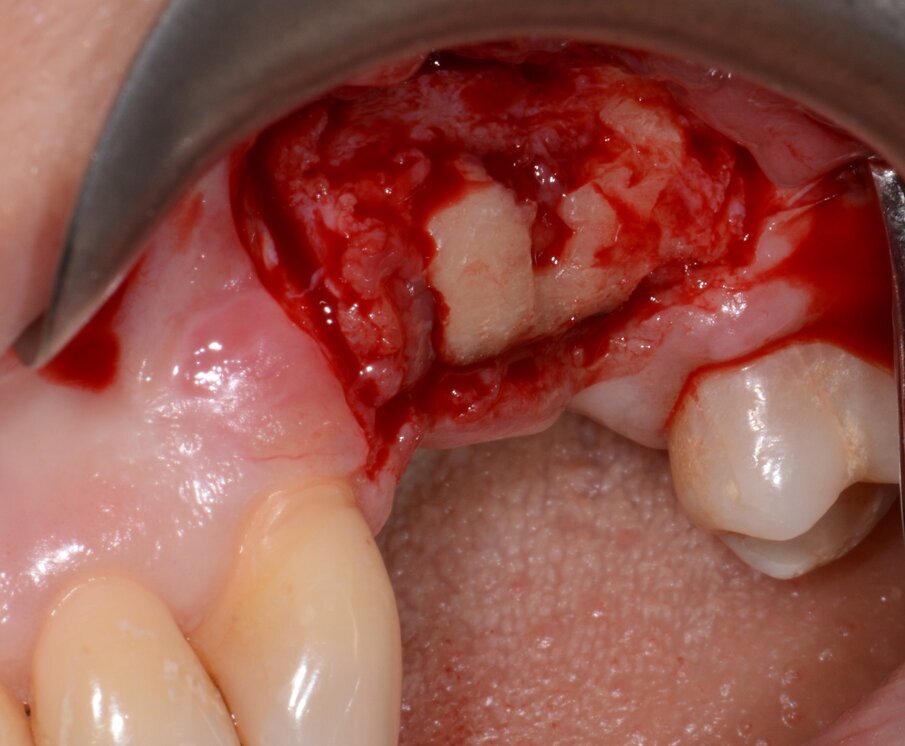
Fig. 11: Bone augmentation
Fig. 12: Final results with restoration two years post-op.
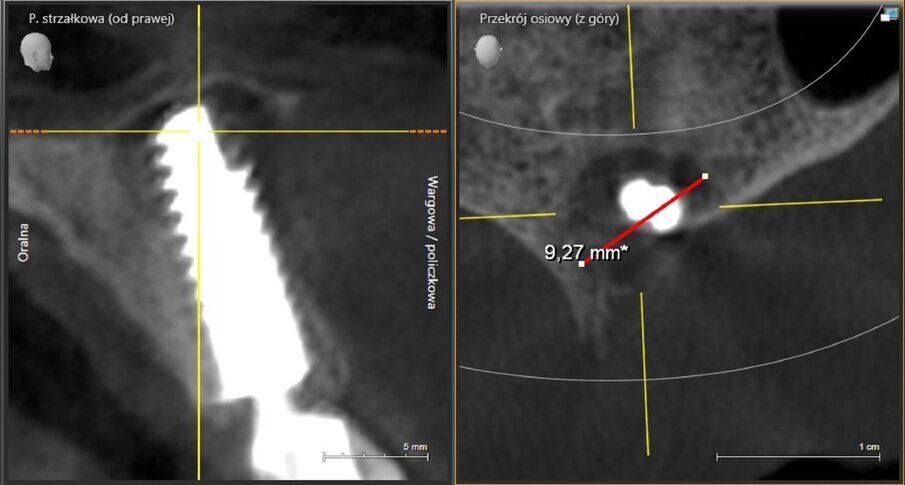
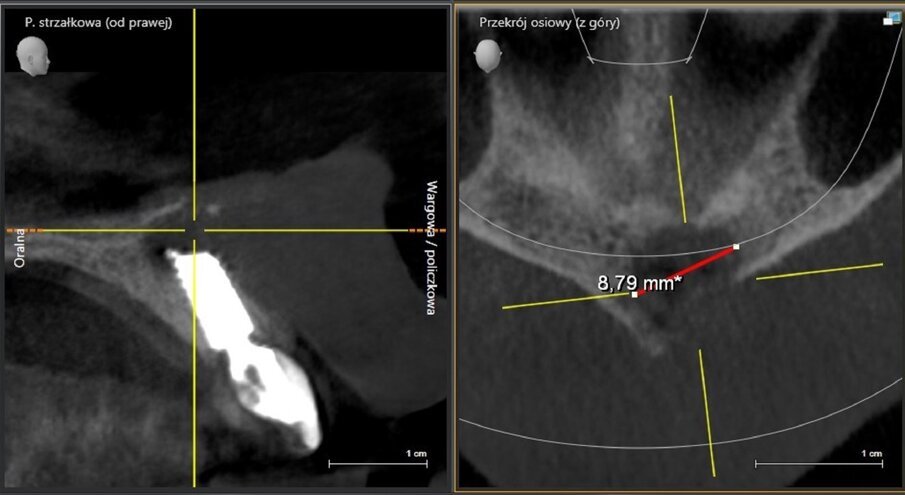
The implant apicectomy in Case 3 shows that one year after the immediate implantation with immediate loading there was inflammation around the implant apex. The rest was properly integrated (Figs. 13–20).
Fig. 13: Initial situation. Visible fistula one year after loading.
Fig. 14: Bone defect of 9.27mm in diameter.
Fig. 16: Granulation tissue removal with Er:YAG.
Fig. 17: Implant resection.
Fig. 18: CBCT scan on the day of surgery. No bone augmentation.
Fig. 19: CBCT scan 1.5 years post-op. Visible bone regeneration.
Fig. 20: Situation 1.5 years post-op. No sign of inflammation.
What advice would you give to your dental colleagues who may be considering whether to incorporate laser technology into their practice?
I can only advise them to use laser; there is no reason to hesitate. Laser technology really changes dental practice. Laser use provides new possibilities, new treatment protocols and many advantages in dental procedures. Our treatments are more comfortable, less painful (sometimes even painless) and very often less invasive and more predictable. We have a great advantage of selective tissue removal based on the chosen laser wavelength and settings. Last but not least, it is better for our marketing, and patients now expect newer technologies.
Tags:
Pulsed Nd:YAG dental lasers are surgical tools used to obtain specific surgical objectives as defined in the LANAP (laser-assisted new attachment procedure)...
MONACO: The zero peri-implantitis concept of the Patent Dental Implant System, designed to prevent disease onset and maintain long-term soft-tissue health, ...
Peri-implantitis continues to be one of the greatest challenges for dental professionals. According to studies, the prevalence of the condition will ...
Late implant failure, particularly in the aesthetic zone, presents significant clinical and biological challenges. This case report describes a digitally ...
VIENNA, Austria: Regedent is marking a major milestone at EuroPerio11 with a symposium highlighting ten years of clinical experience with hyaDENT BG, a ...
Conducted in collaboration with the Medical University of Graz in Austria, a new long-term study with over five and up to 12 years of follow-up found no ...
Nowadays, virtual planning and the assisted placement of implants in 3-D positions relative to the bone, soft tissue and final planned prosthesis are ...
VIENNA, Austria: According to a large-scale study review by Derks et al.,¹ one in five implant patients develops peri-implantitis, and nearly twice as many...
Pulpal exposures are unfortunately a routine occurrence when treating carious teeth and frequently lead to endodontic treatment owing to the size of the ...
VICENZA, Italy: Peri-implant disease poses a significant challenge in implantology. Recognising the need for a more effective and systematic approach to ...
Live webinar
Wed. 28 January 2026
8:00 am EST (New York)
Live webinar
Wed. 28 January 2026
11:00 am EST (New York)
Prof. Dr. Jan-Frederik Güth
Live webinar
Wed. 28 January 2026
11:00 am EST (New York)
Dr. Algimante Lošytė – Jančė
Live webinar
Wed. 28 January 2026
12:00 pm EST (New York)
Live webinar
Wed. 28 January 2026
1:00 pm EST (New York)
Dr. Marina Siegenthaler Dr. med. dent. eidg. dipl. Zahnärztin SSO
Live webinar
Thu. 29 January 2026
1:00 pm EST (New York)
Live webinar
Thu. 29 January 2026
8:00 pm EST (New York)



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East
























































To post a reply please login or register