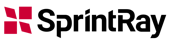
Recently, semi-occlusive or fully occlusive CAD/CAM titanium meshes have also been introduced, and they have shown similarly favourable results.10–12 From a histological, histo-morphometric and micro-CT perspective, the bone tissue regenerated using these meshes has shown more than adequate characteristics for achieving osseointegration,13–15 especially for the long-term maintenance of implants under functional loading.16
Another important innovation is the double-layer closure technique based on the use of the buccal pad of fat for areas subjected to vertical GBR. This technique has significantly reduced the rate of exposure and infection, consequently increasing the success of GBR.17
This case report aims to illustrate, step by step, the treatment of a severe bone defect located in the upper jaw using a customised CAD/CAM titanium mesh combined with the buccal pad of fat, and the subsequent implant and prosthetic treatment using computer-guided surgery, in order to show how new technologies and digital workflows can simplify the treatment of complex cases.
Case report
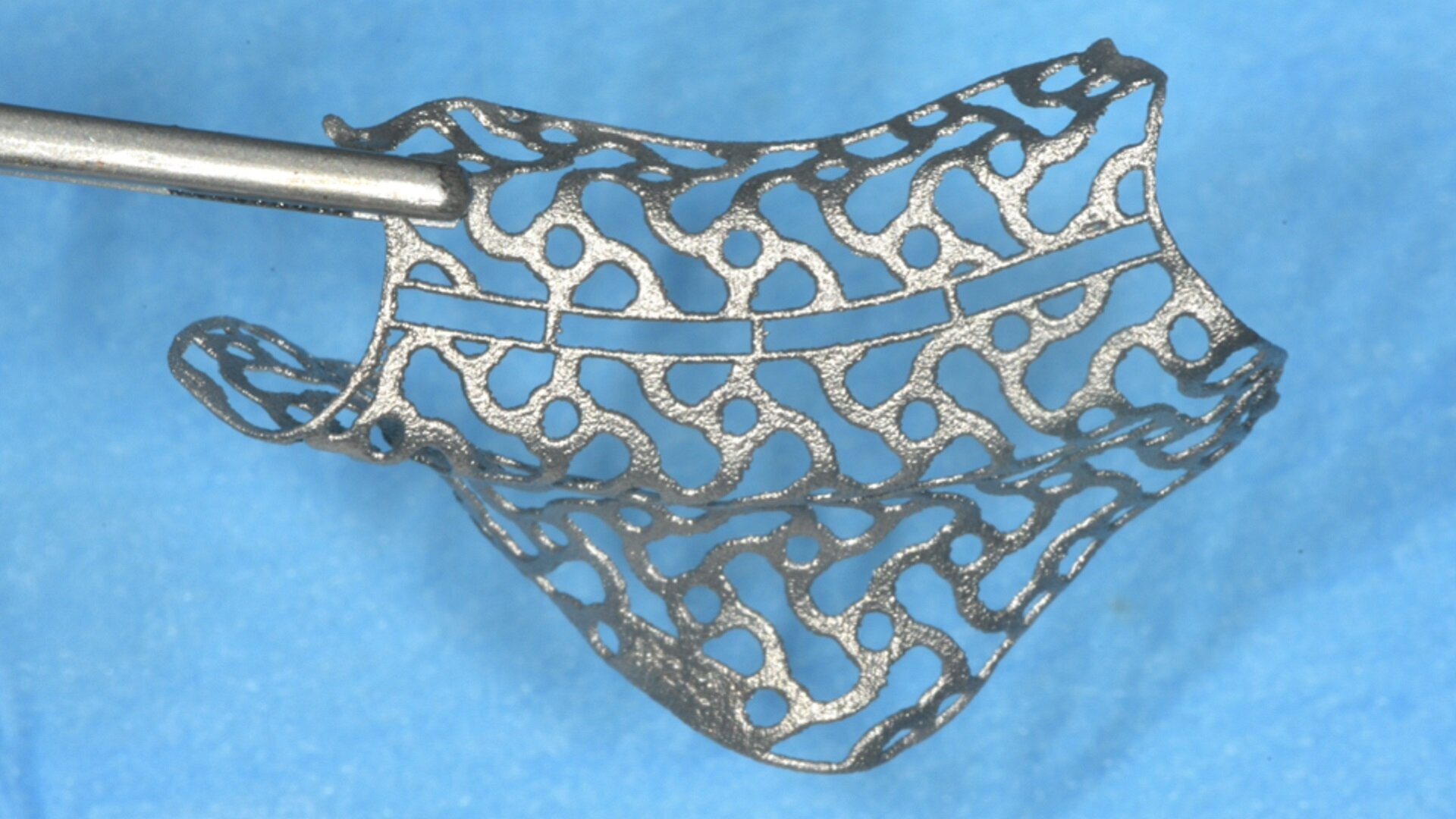
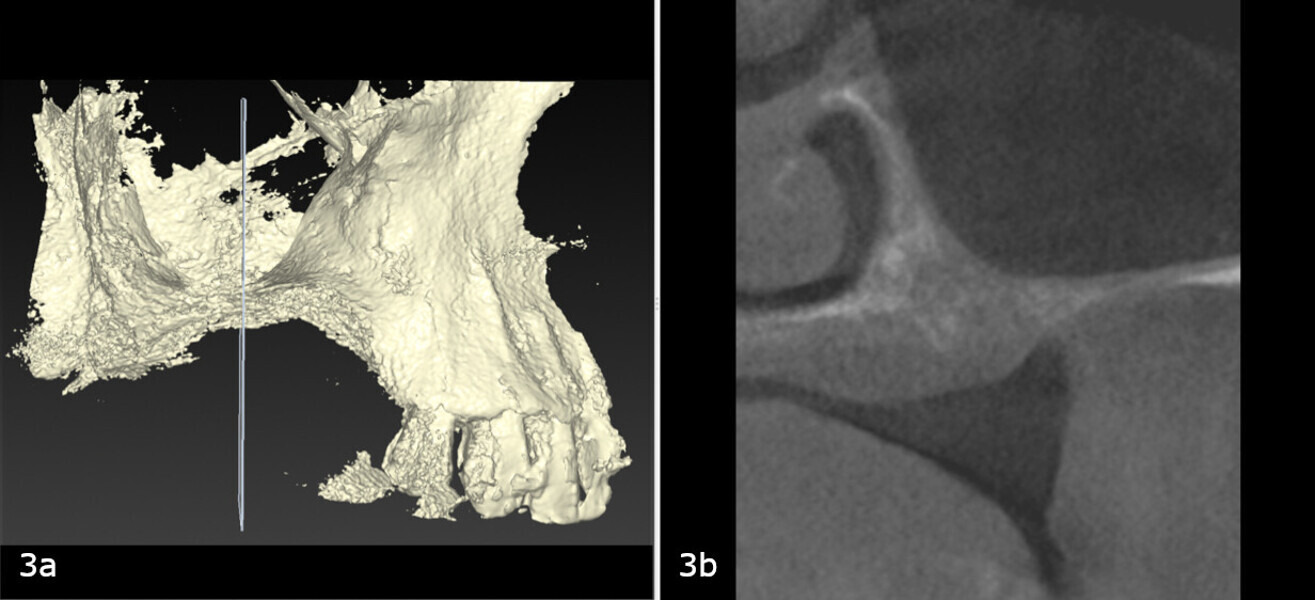
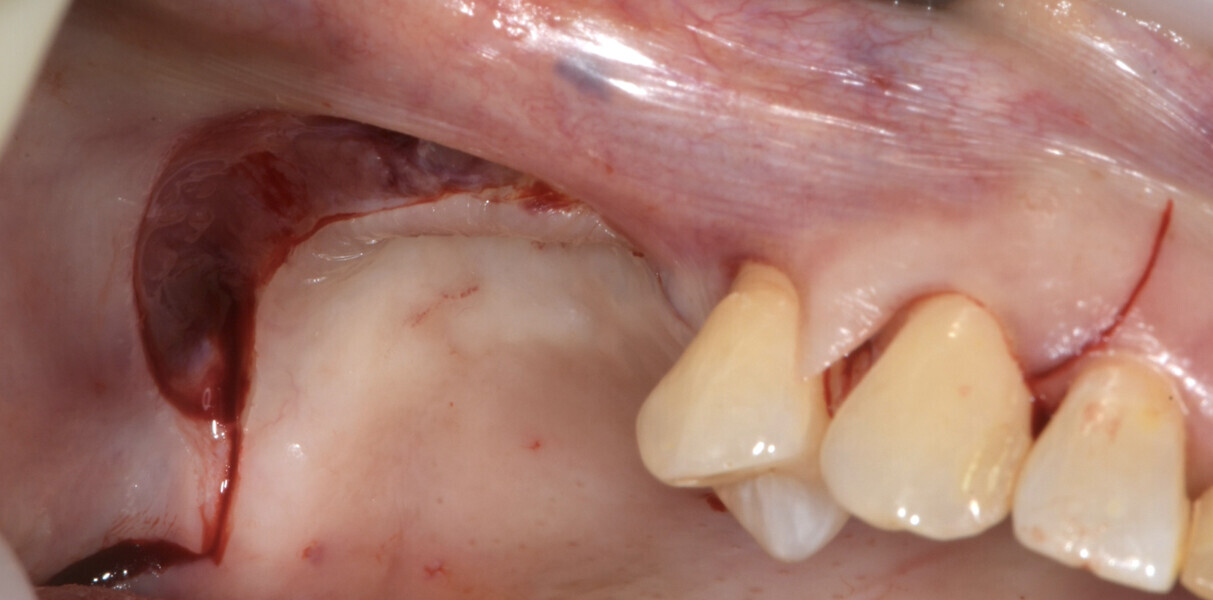
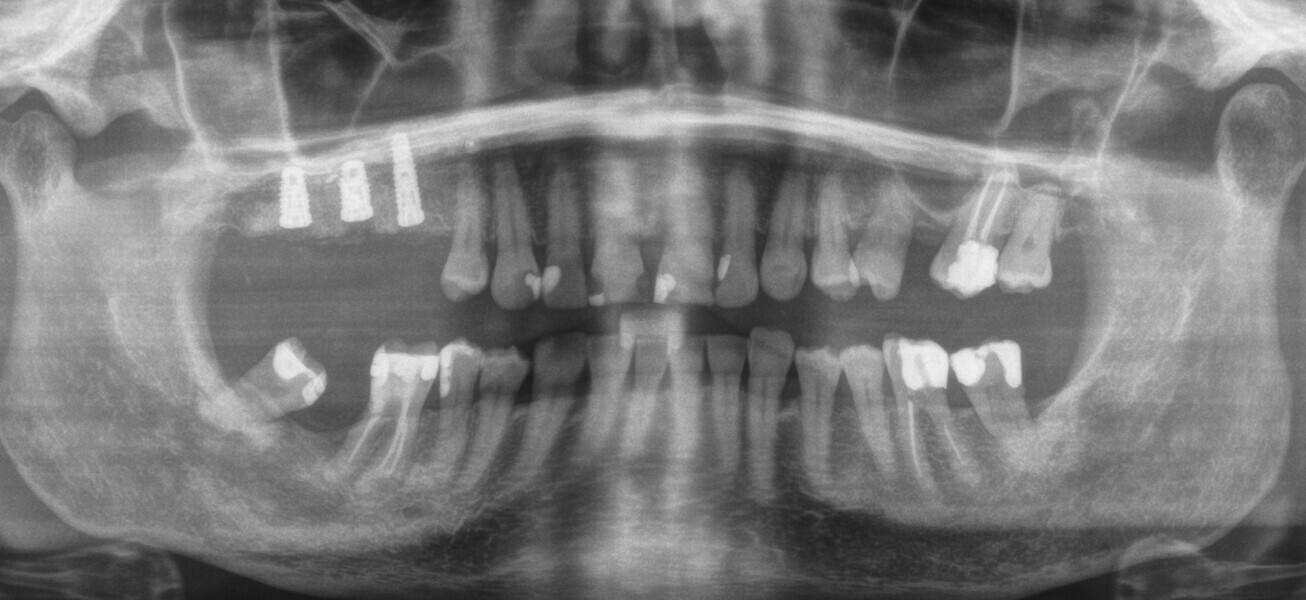
A 62-year-old female patient (ASA Class I), a non-smoker and with normal glucose levels, with previously treated periodontal disease presented for implant and prosthetic rehabilitation of the upper jaw (Fig. 1). Radiographic analysis, performed through a dental panoramic tomogram and CBCT scan, revealed the presence of a vertical bone defect in the right posterior sextant, due to the complete loss of the alveolar process (Figs. 2; 3a & b). The clinical examination showed the severity of the bone defect, which had resulted in an obvious volume deficiency in both the horizontal and vertical dimensions (Figs. 4 & 5).
After discussing the treatment options with the patient, the first-choice treatment was accepted. This would involve the reconstruction of the alveolar process and subsequent rehabilitation with single crowns on implants.
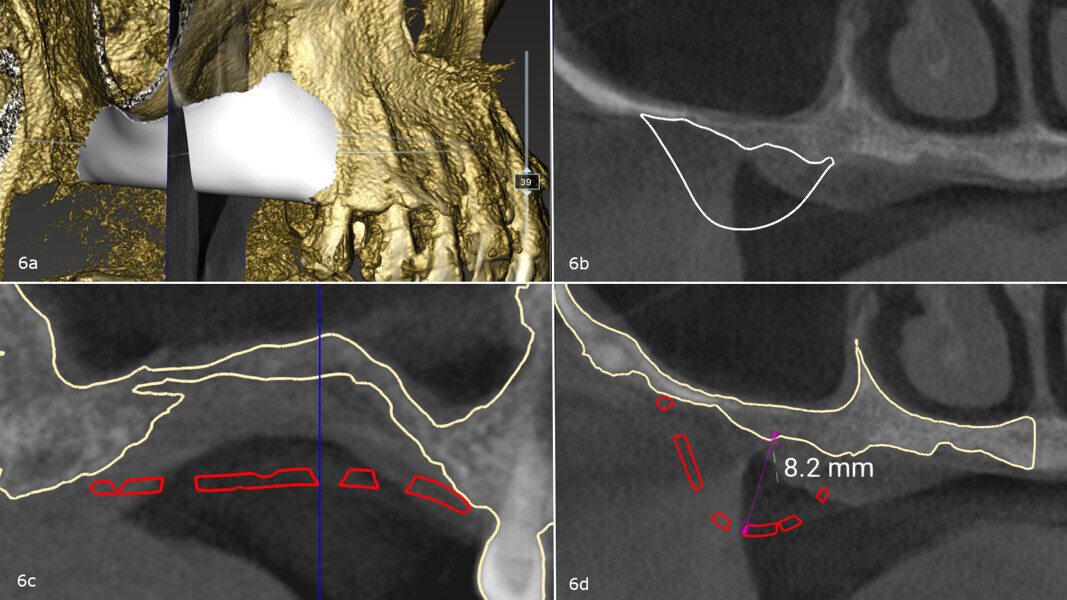
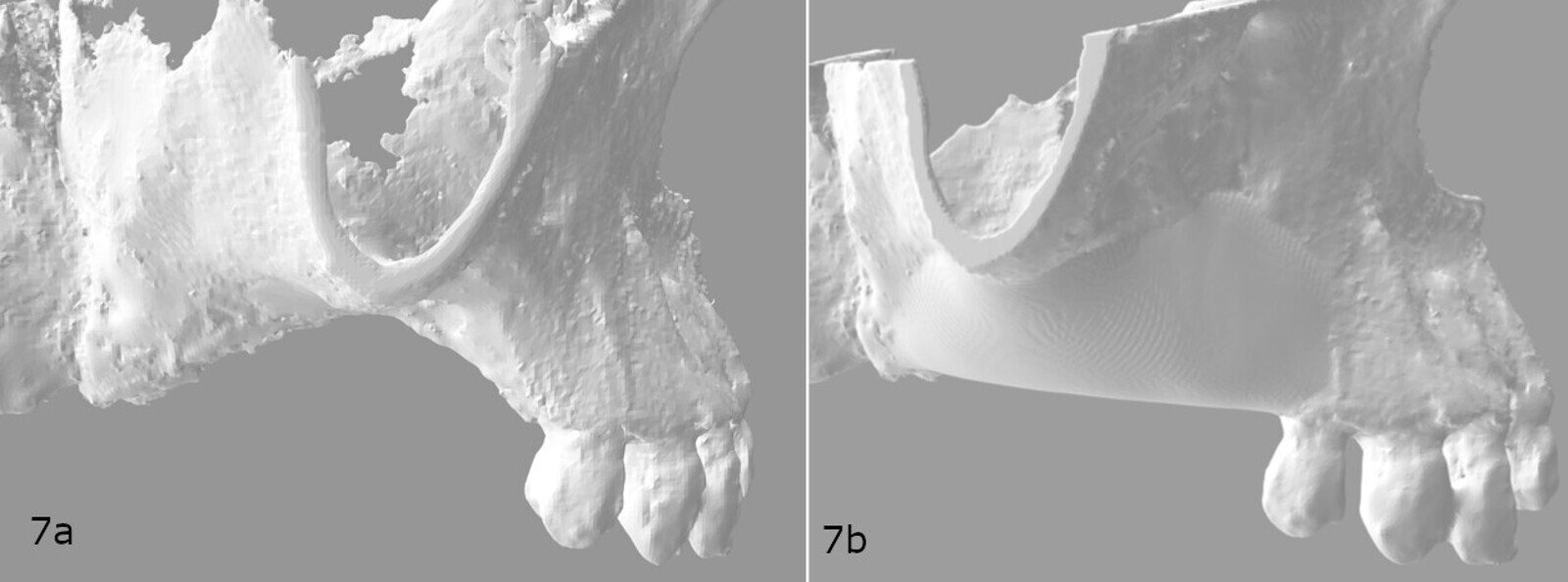
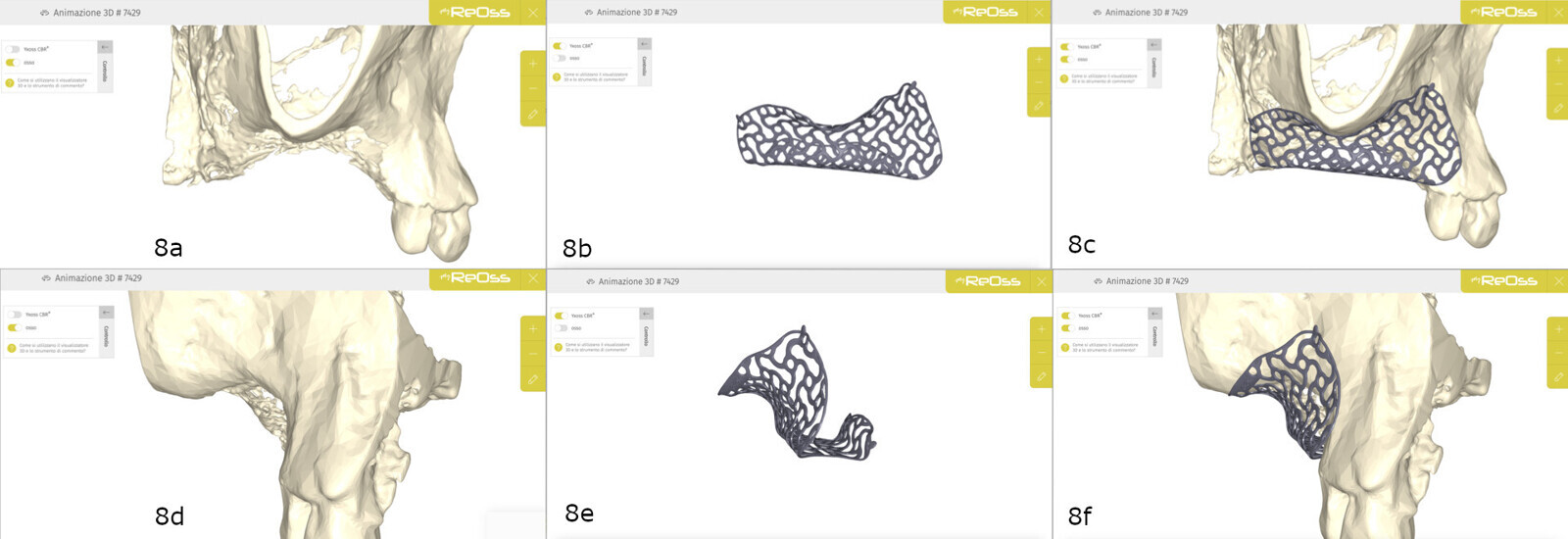
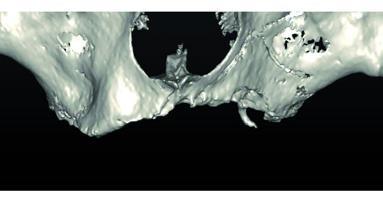
The treatment plan was developed using a fully digital workflow. The DICOM files obtained from the preoperative CBCT scan were used to generate a 3D reconstruction of the maxilla, which allowed for the virtual design of the ideal bone volume for the placement of three implants in sites #15, 16 and 17 (Figs. 6a-d; 7a & b). Subsequently, the customised mesh corresponding to the increased volume in the patient’s maxilla was created virtually (Figs. 8a-f).
On the day of the reconstructive surgery, antibiotic prophylaxis (2 g of amoxicillin with clavulanic acid and 500 mg of metronidazole), anti-inflammatory prophylaxis (20 mg of piroxicam), oral cavity disinfection (oral rinsing with povidone-iodine for 1 minute, hydrogen peroxide for 2 minutes and a 0.2% chlorhexidine mouthwash for 3 minutes) and conscious sedation (2 ml of delorazepam and 2 ml of diazepam) were performed, along with local anaesthesia using 4% articaine and 1:100,000 adrenaline.18
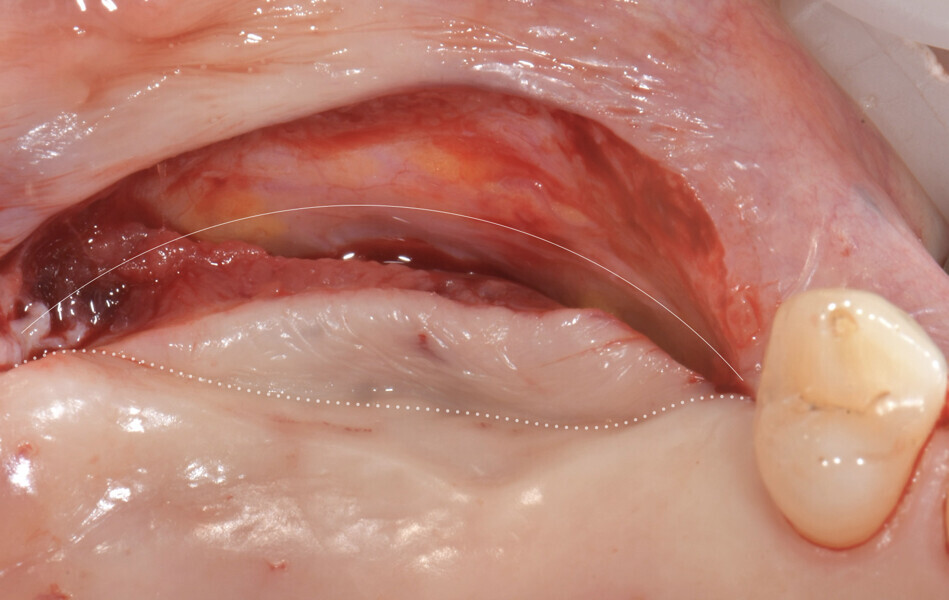
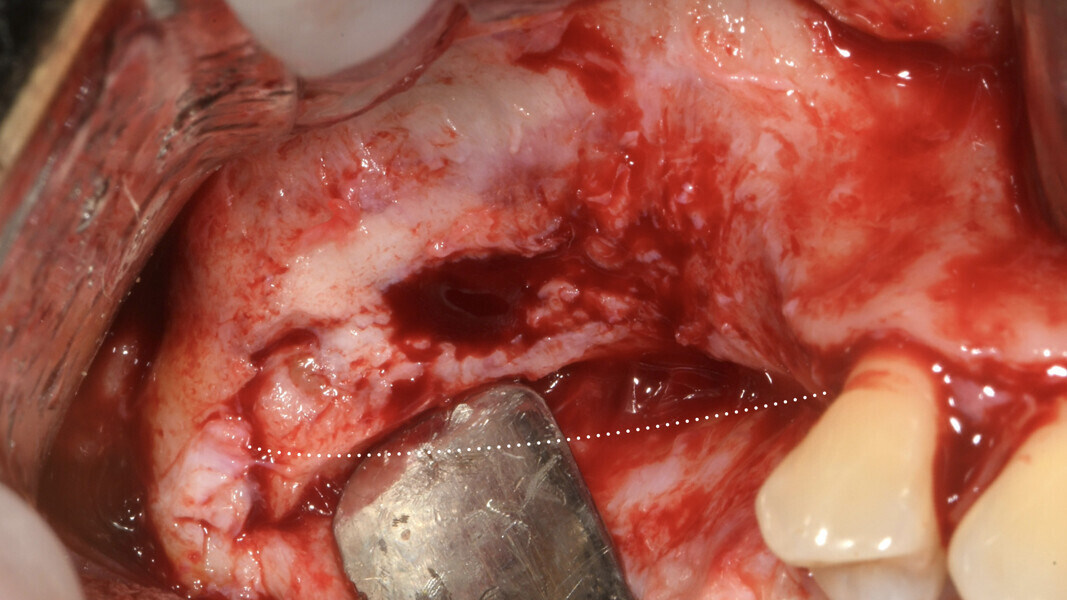
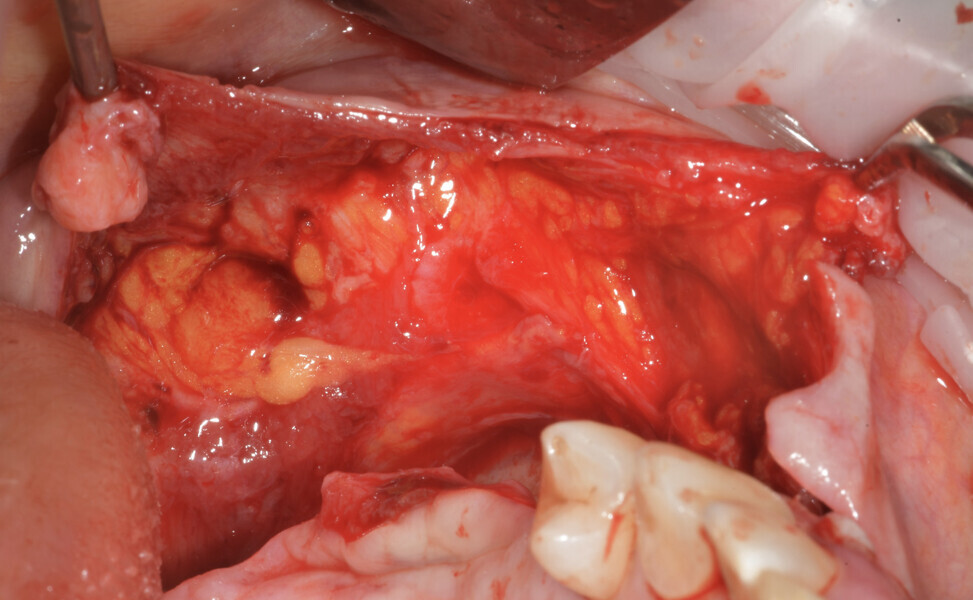
The surgery began with a semilunar incision into the alveolar mucosa on the buccal side of the area to be treated, associated with two vertical vestibular incisions (Figs. 9 & 10).19 A full-thickness flap was then elevated on the buccal side and subsequently mobilised with a periosteal incision, followed by a superficial dissection to separate the mucosal layer from the underlying muscle (Figs. 11 & 12). A full-thickness flap was also elevated on the palatal side, isolating the greater palatine artery (Fig. 13).
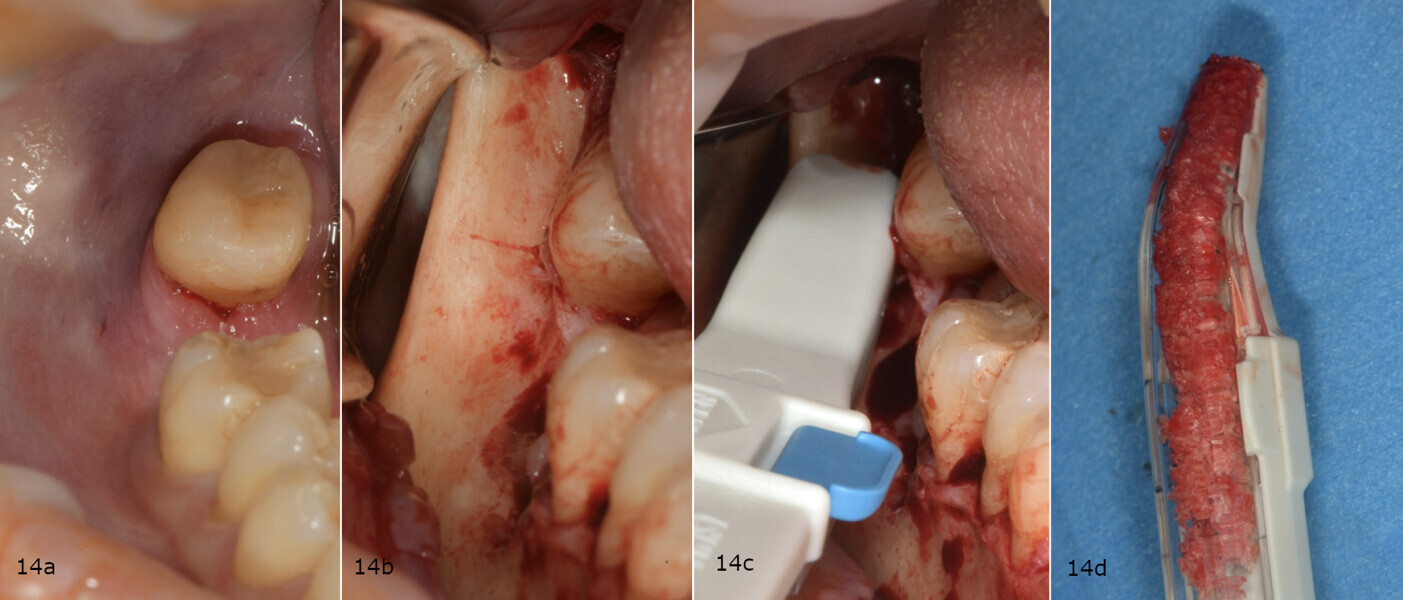
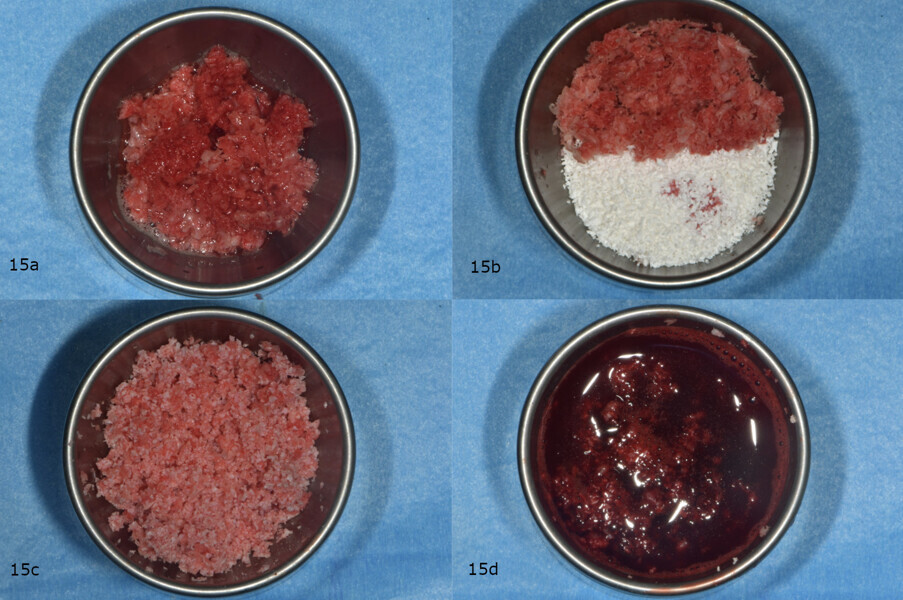
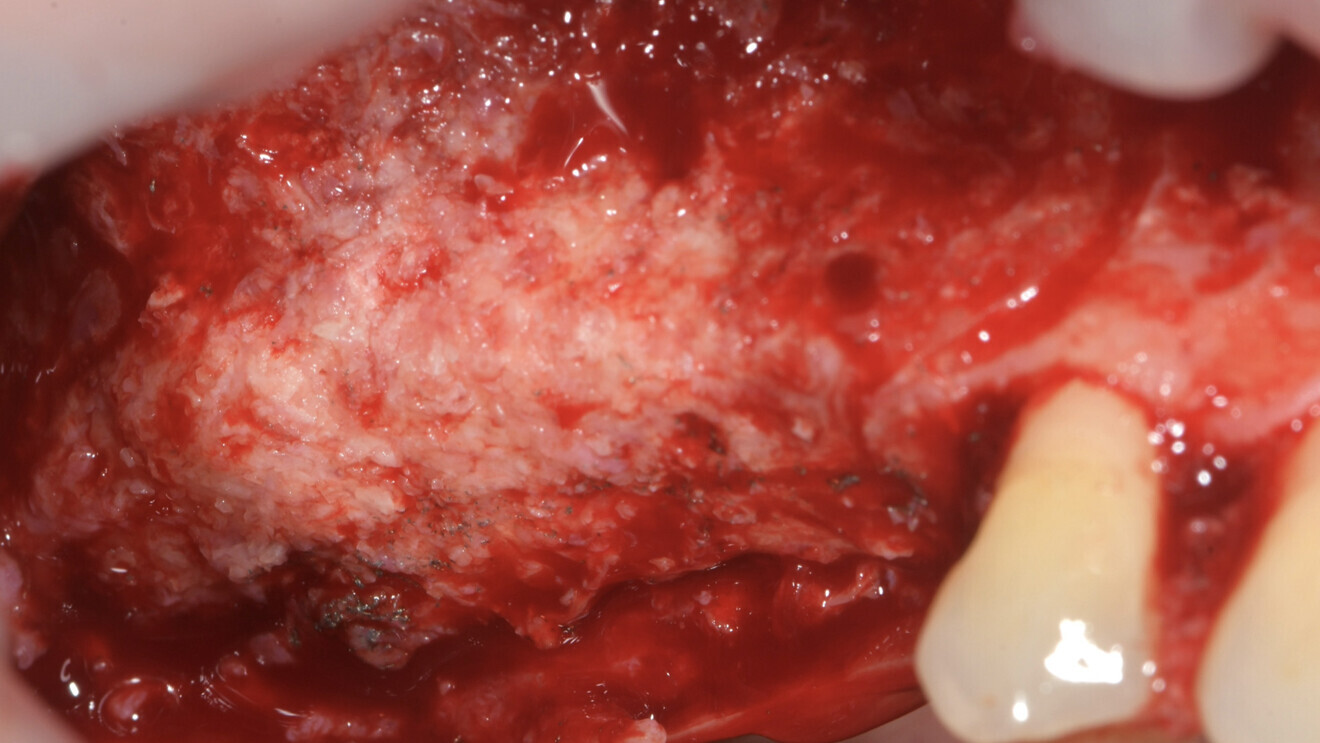
A horizontal incision was made along the mandibular ramus to harvest about 2 cm3 of autologous bone using a bone scraper (SafeScraper TWIST, Meta Technologies; Fig. 14a-d). The grafting material was then prepared by mixing a 50:50 ratio of autologous bone to deproteinised bovine bone matrix (Geistlich Bio-Oss, small granules), to which peripheral venous blood taken from the patient was added to promote coagulation (Figs. 15a-d).
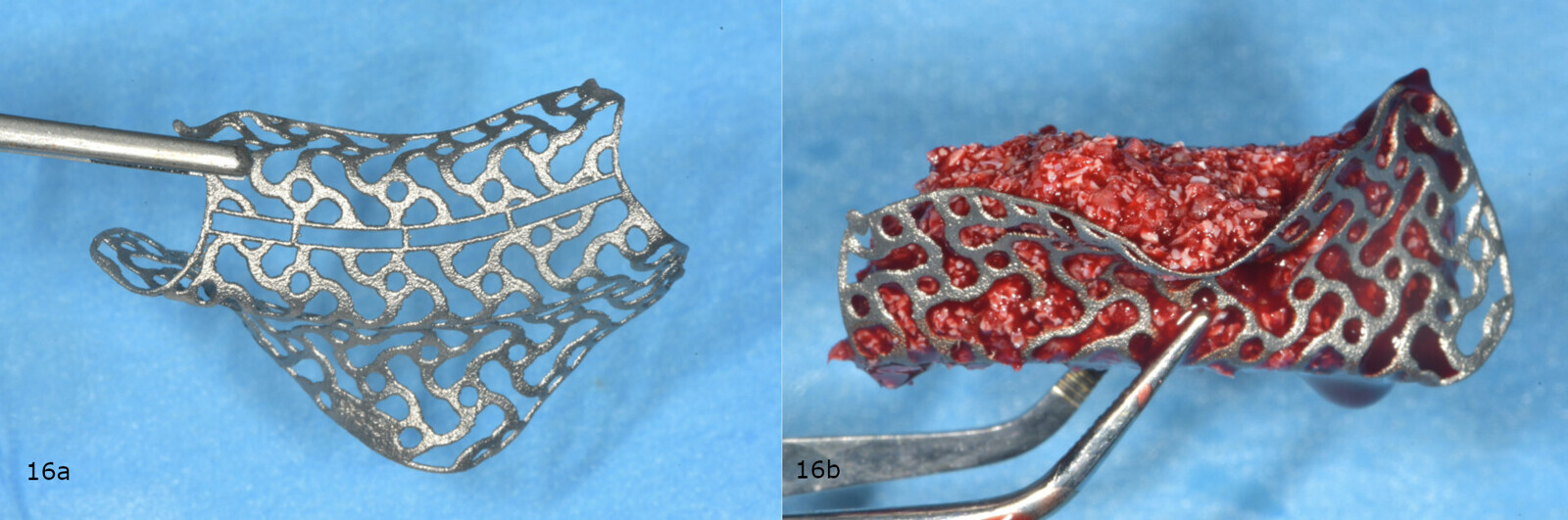
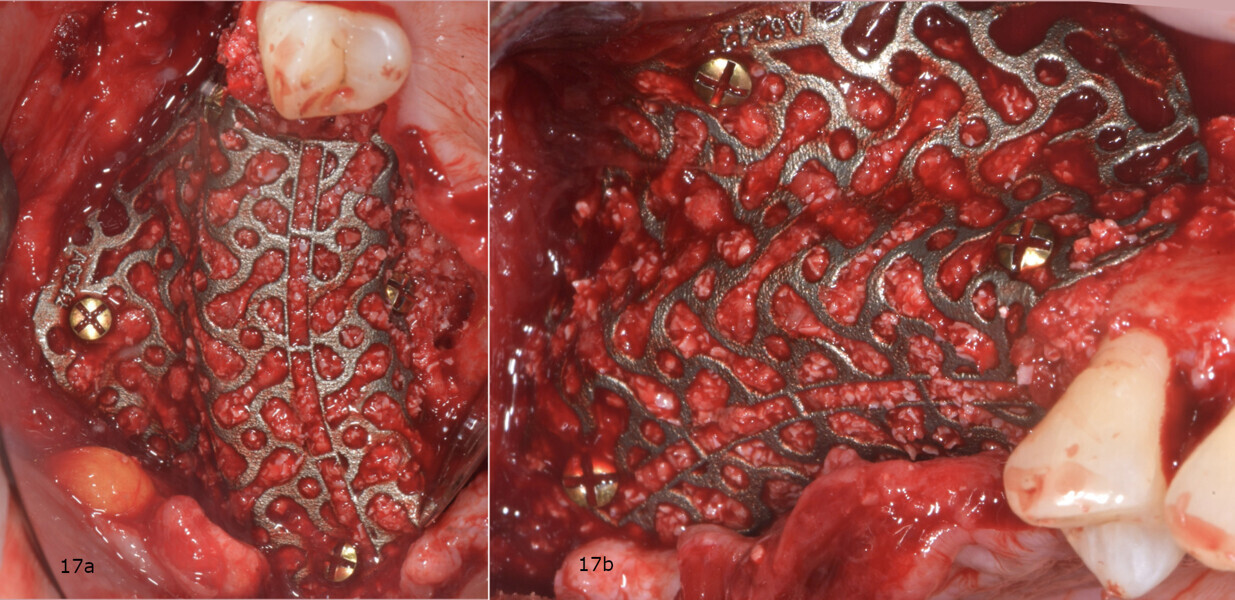
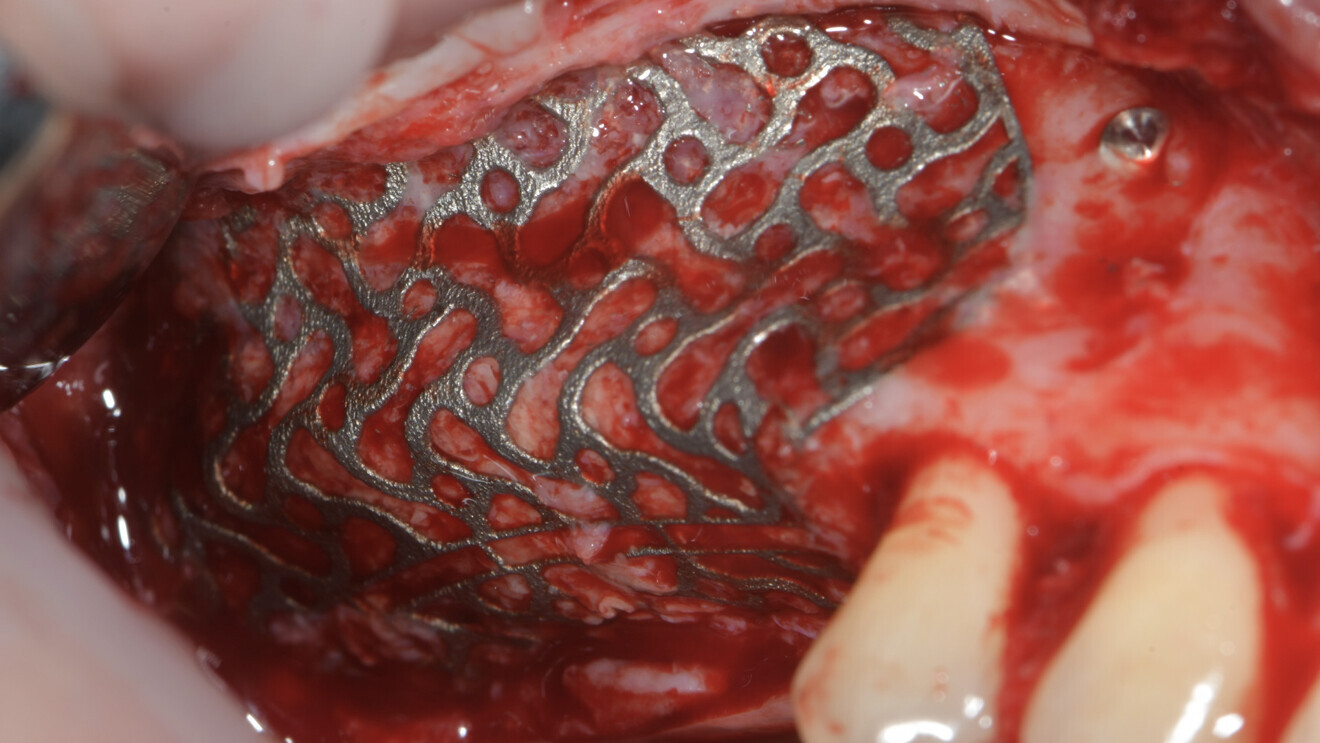
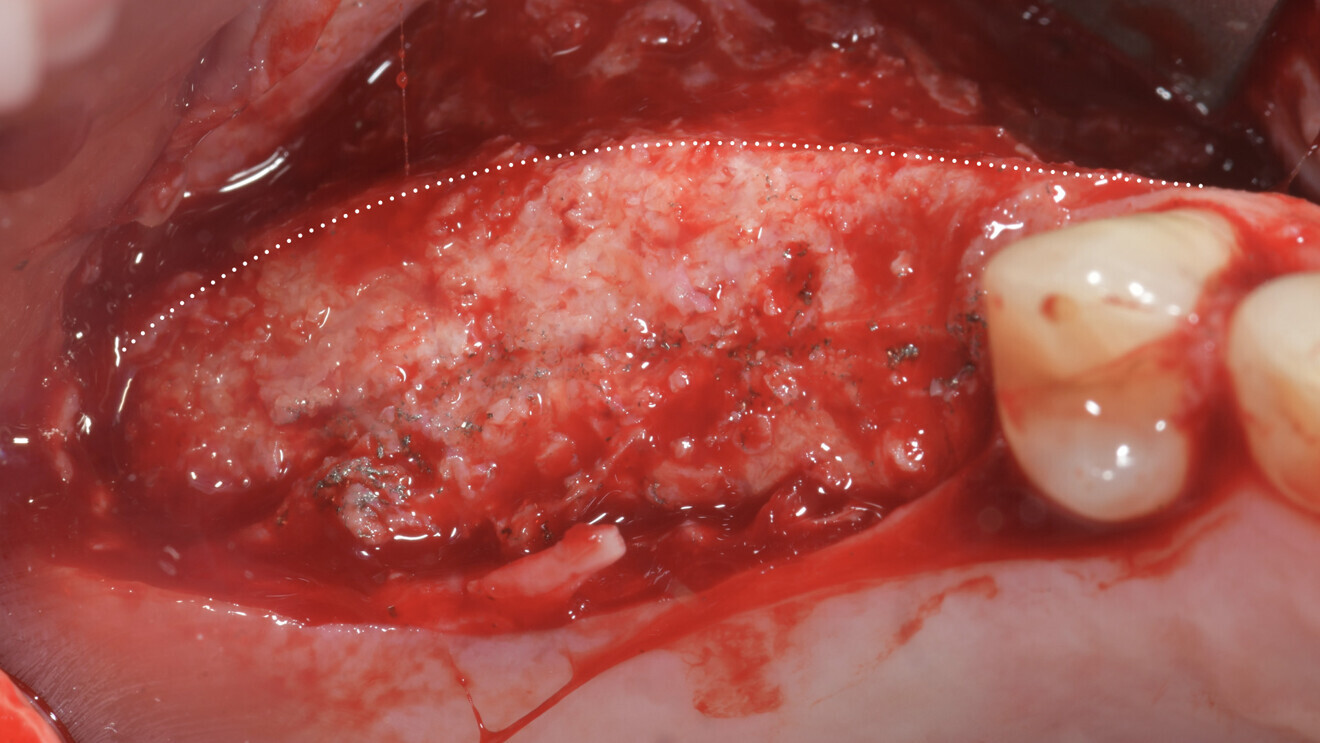
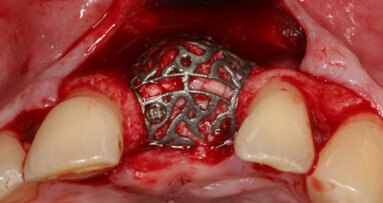
Subsequently, the customised CAD/CAM titanium mesh (Yxoss CBR, ReOss) was taken from the double sterile pouch and filled with the grafting material (Figs. 16a & b). The mesh was then positioned in place and fixed with four osteosynthesis screws (BT screw, BTK) to achieve absolute stability (Figs. 17a & b). It was then covered with a native collagen resorbable membrane (Geistlich Bio-Gide), which was stabilised with titanium tacks (MCbio, Geistlich; Fig. 18).
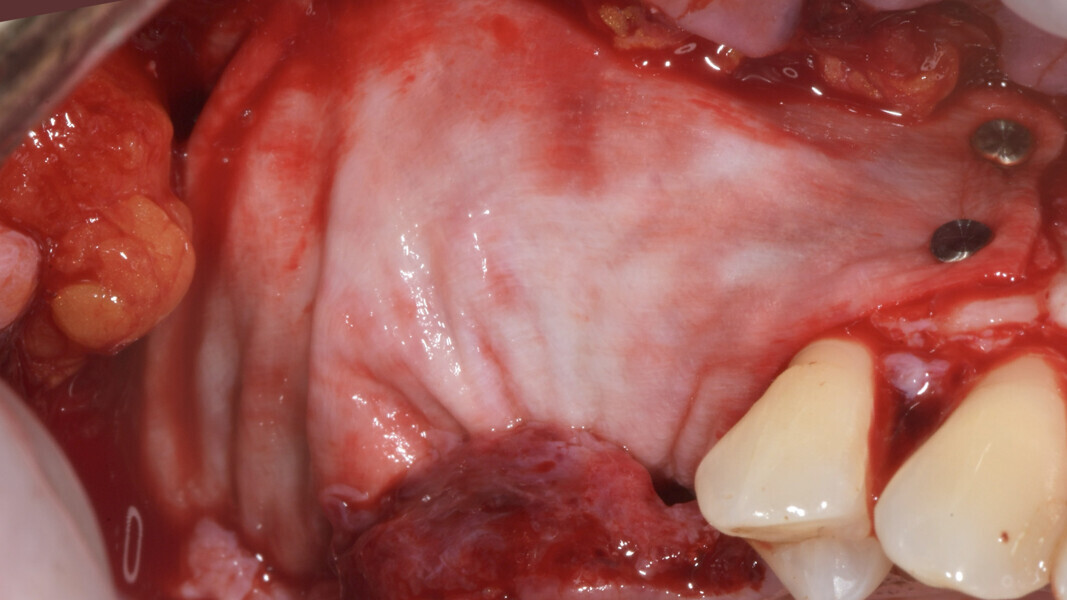
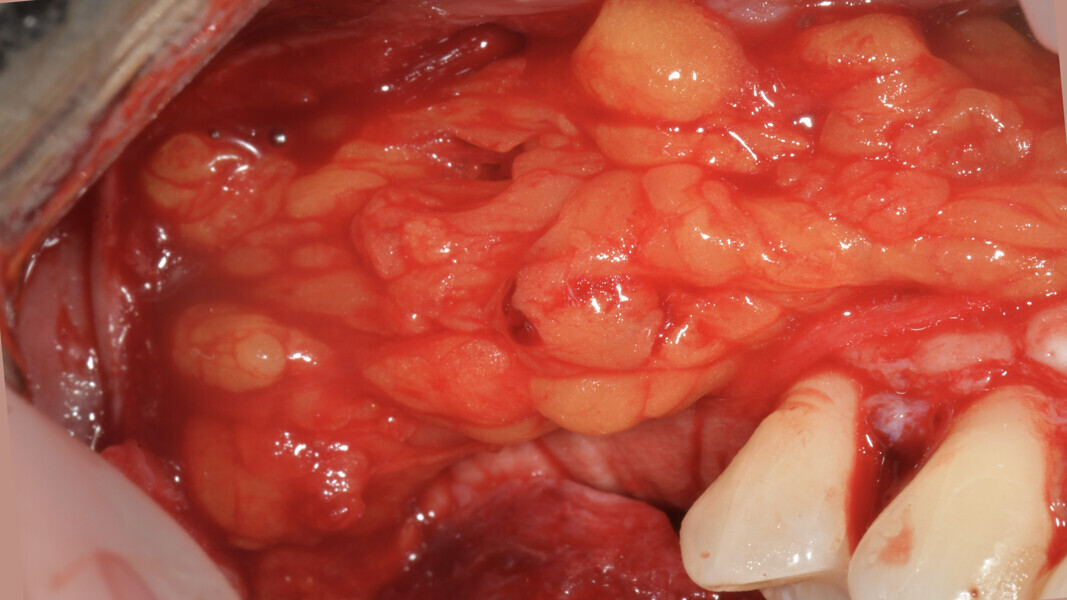
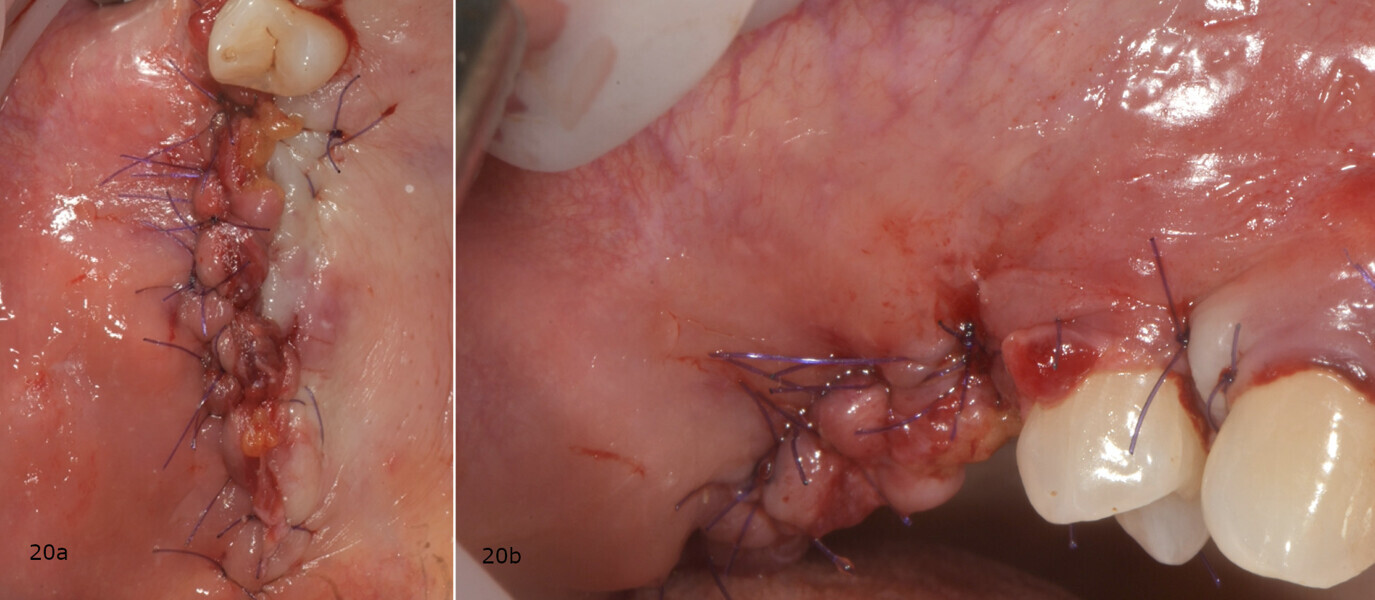
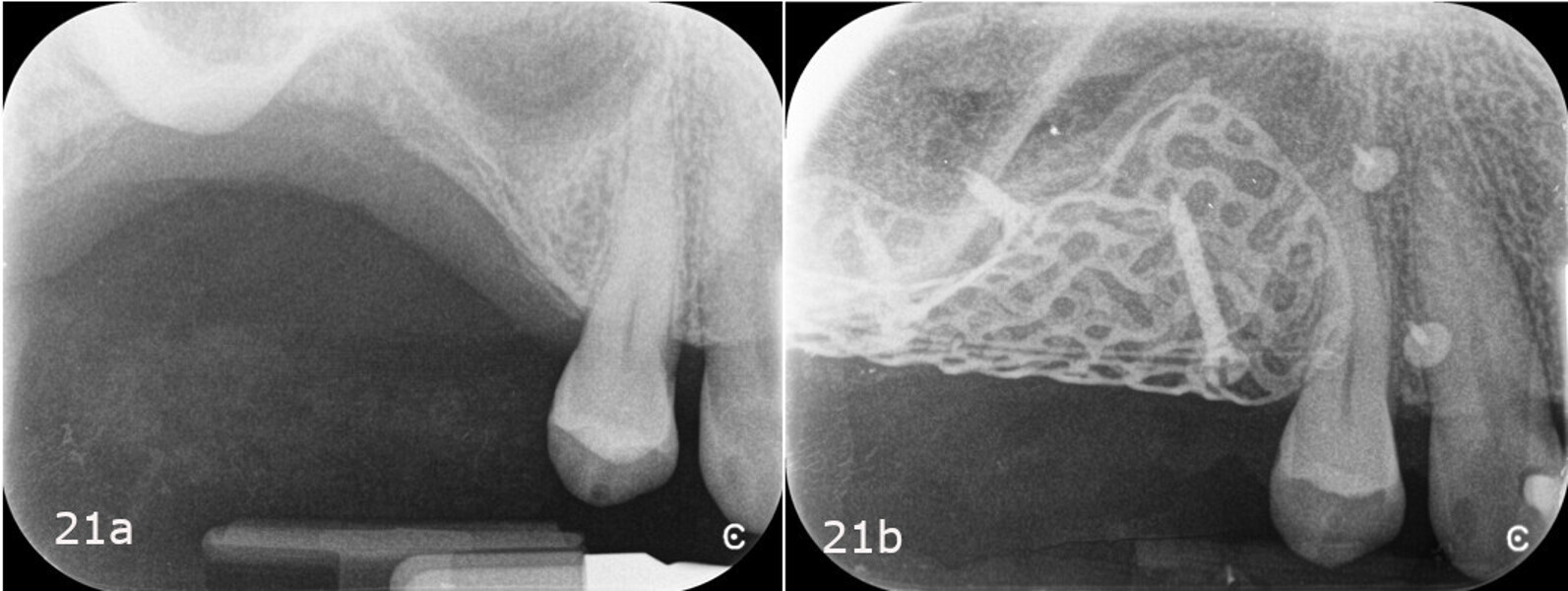
As it is a tissue extremely rich in pluripotent cells, capable of differentiating to promote healing by first intention of the treated area, the buccal pad of fat was isolated and advanced before closing the primary flap to reduce the risk of exposure and infection of the underlying mesh (Fig. 19).17 Finally, the buccal and vestibular surgical flaps were sutured using a double line of sutures, the first consisting of horizontal mattress sutures and the second of single or double interrupted sutures (GLYCOLON, Resorba; Figs. 20a & b; 21a & b).
After surgery, the patient followed a postoperative protocol that included antibiotic therapy (1 g of amoxicillin with clavulanic acid and 250 mg of metronidazole every 8 hours for seven days) and oral cavity disinfection with a 0.2% chlorhexidine mouthwash for 2 minutes, three times a day, for 14 days.
After 14 days, the sutures were removed, postoperative data was collected, dehiscence or exposure of the mesh was excluded, and a dental panoramic tomogram was taken (Fig. 22). The patient reported a low level of pain, rated at 0 on a visual analogue scale of 0 to 10, and an average intake of 1.6 tablets of a non-steroidal anti-inflammatory drug per day during the first two weeks. The patient also reported significant swelling, a small external bruise on the face and difficulty opening her mouth. According to the postoperative symptom severity questionnaire, a score of 32 was recorded, indicative of moderate postoperative discomfort.
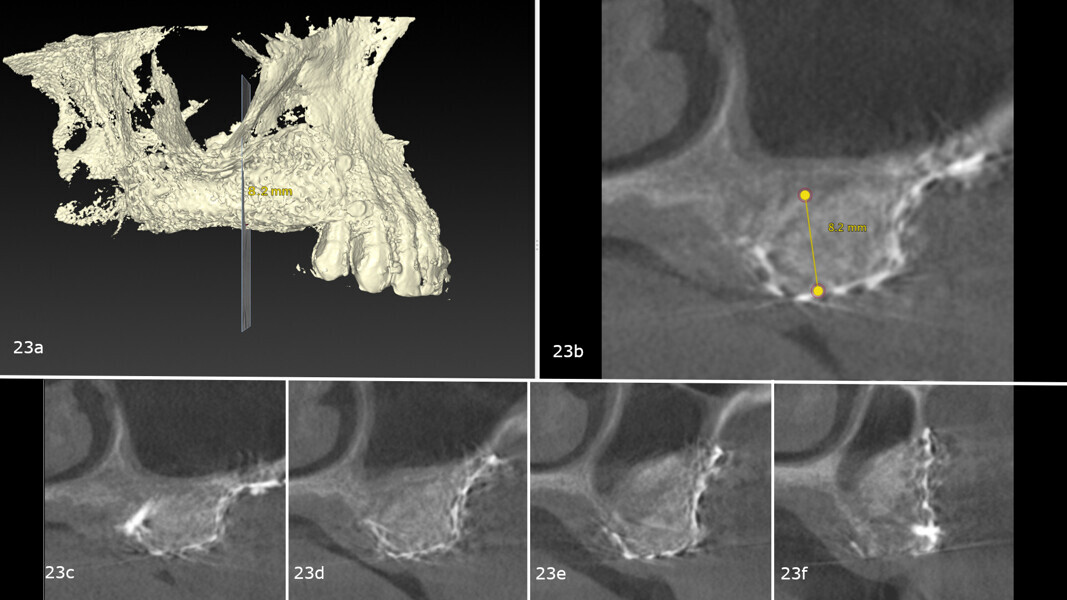
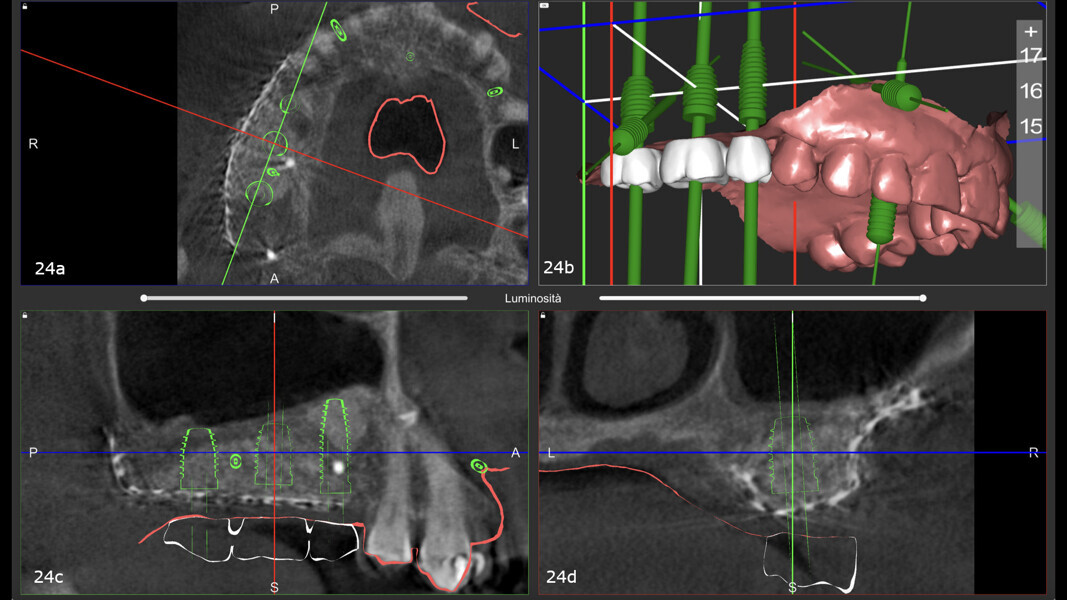
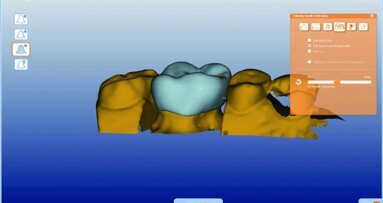
After nine months, a second CBCT scan was performed to assess the regenerated bone volume and plan the computer-guided surgery (Figa. 23a-f). The STL files obtained from the intra-oral scan, and the DICOM files from the CBCT scan were used to plan implant placement through computer-guided surgery (naviMAX, Biomax; Figs. 24a-d).
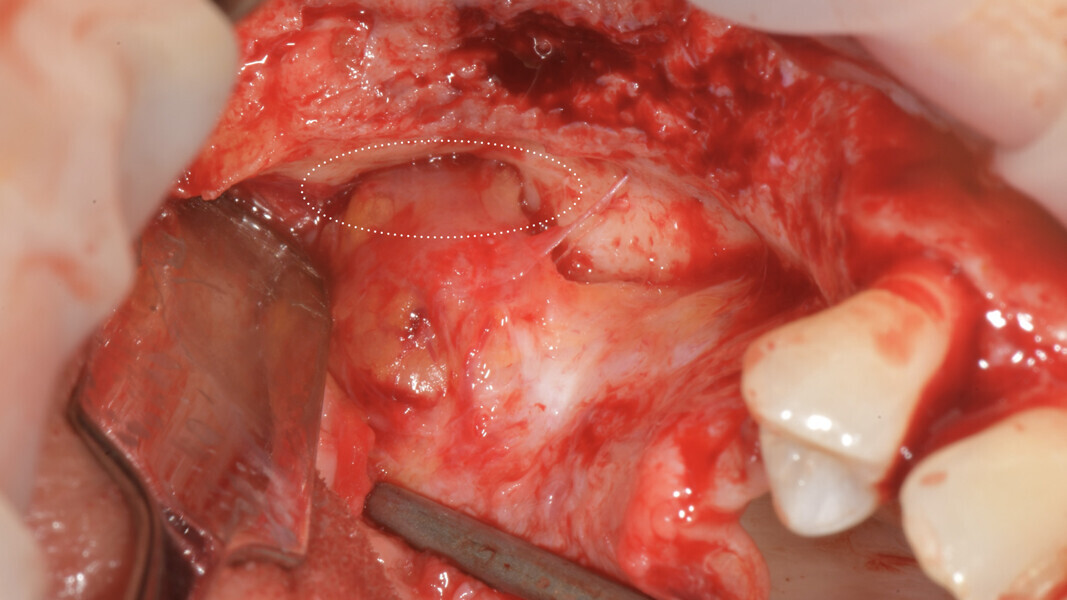
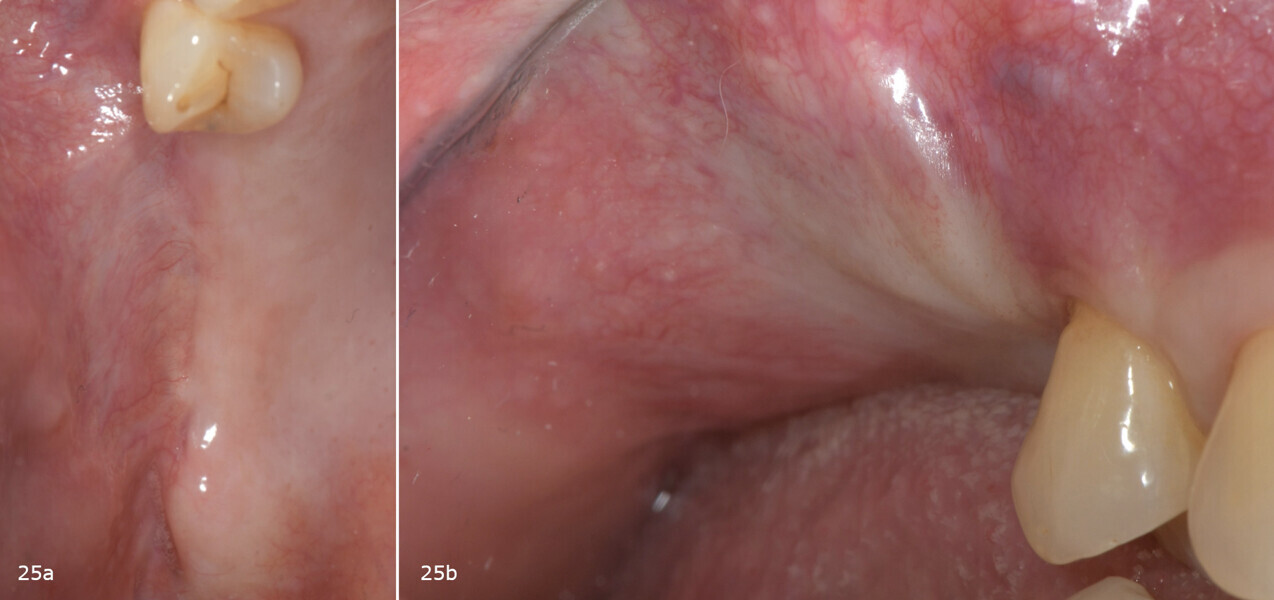
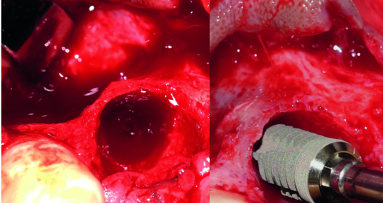
On the day of implant surgery, a para-crestal horizontal incision was made to expose the mesh and remove it, after the removal of the titanium screws and the new bone that had formed over the mesh (Figs. 25a & b, 26). Clinical examination showed complete regeneration of the vertical defect and the absence of pseudo-periosteum or thin pseudo-periosteum (< 1 mm), corresponding to the pseudo-periosteum Type 1 according to the Cucchi classification (Figs. 27 & 28).20
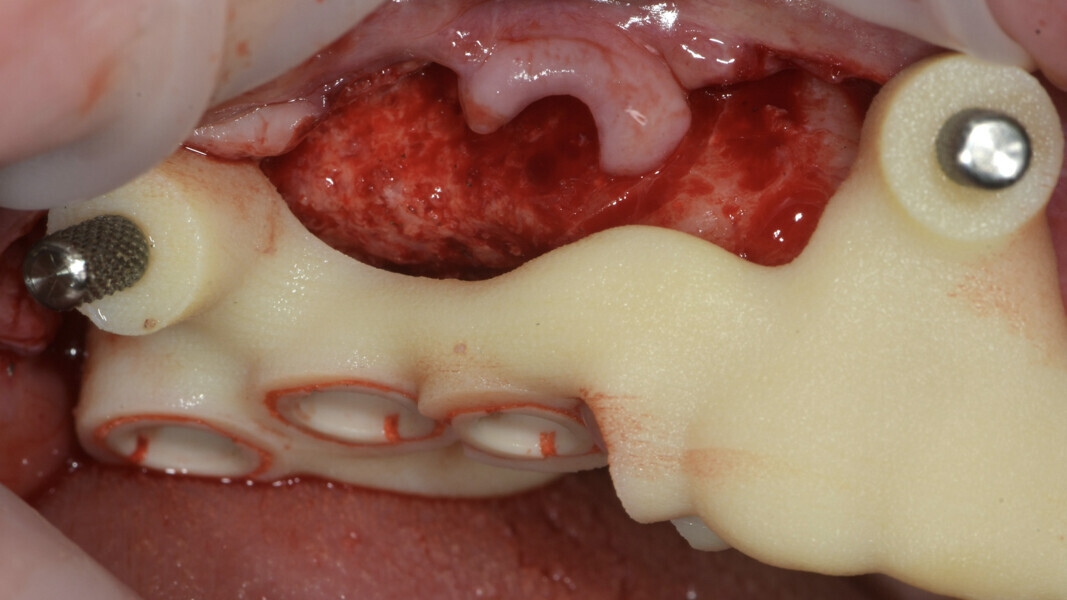
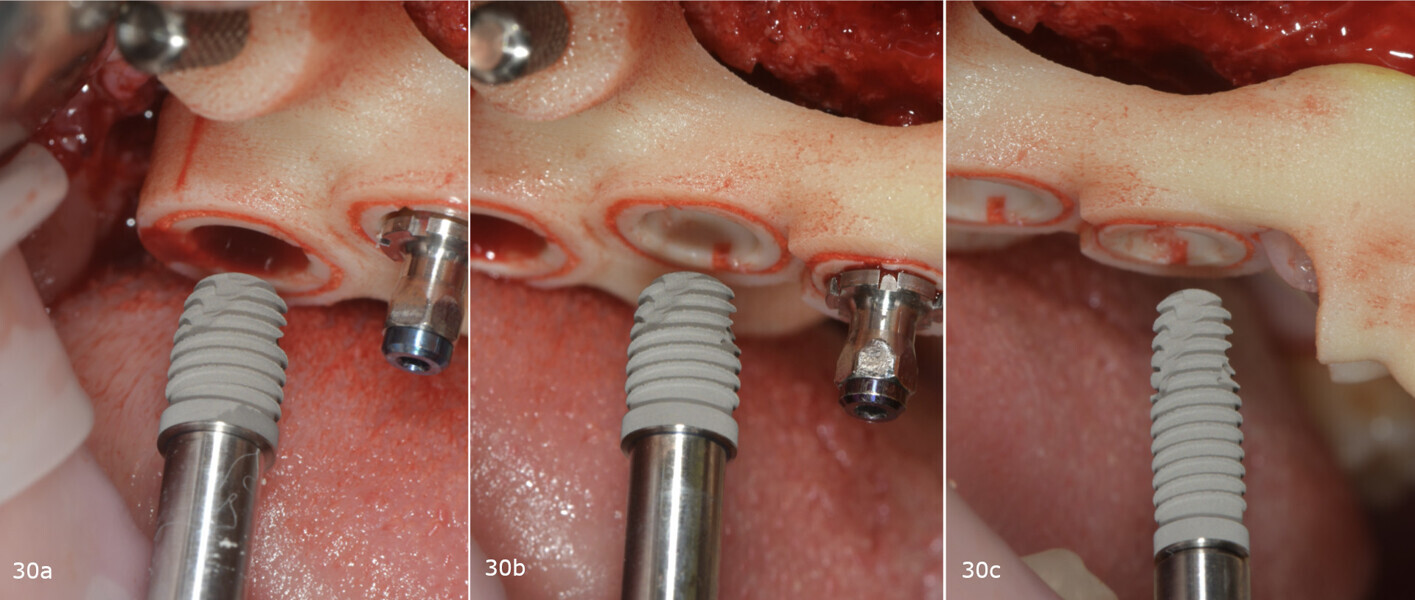
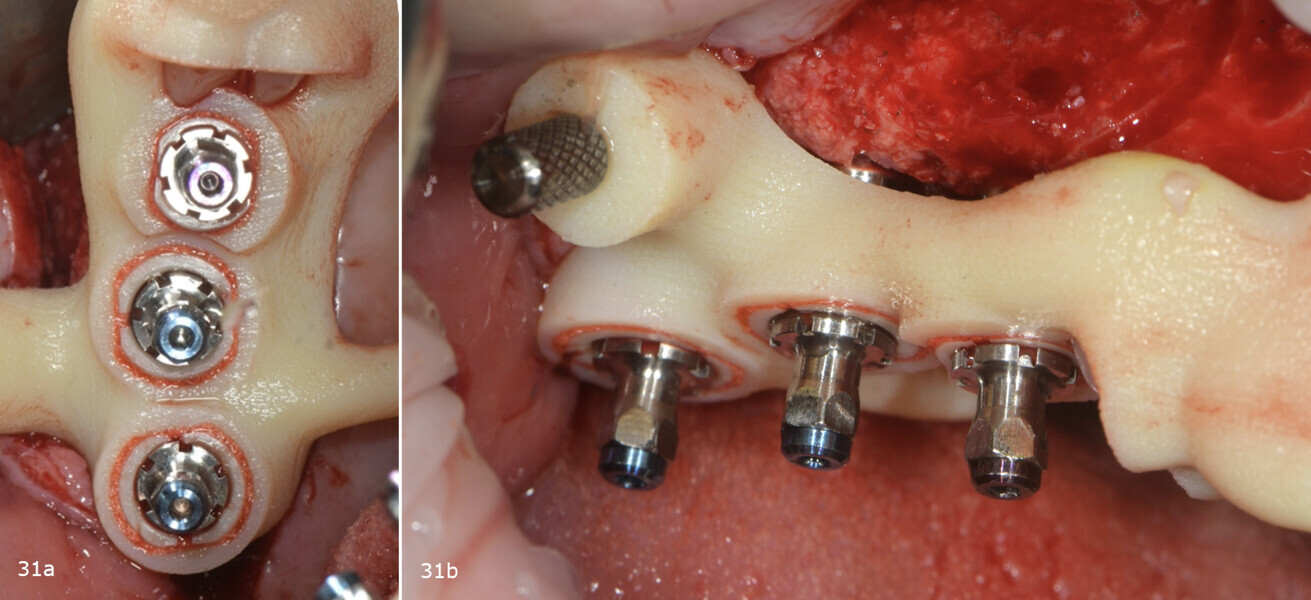
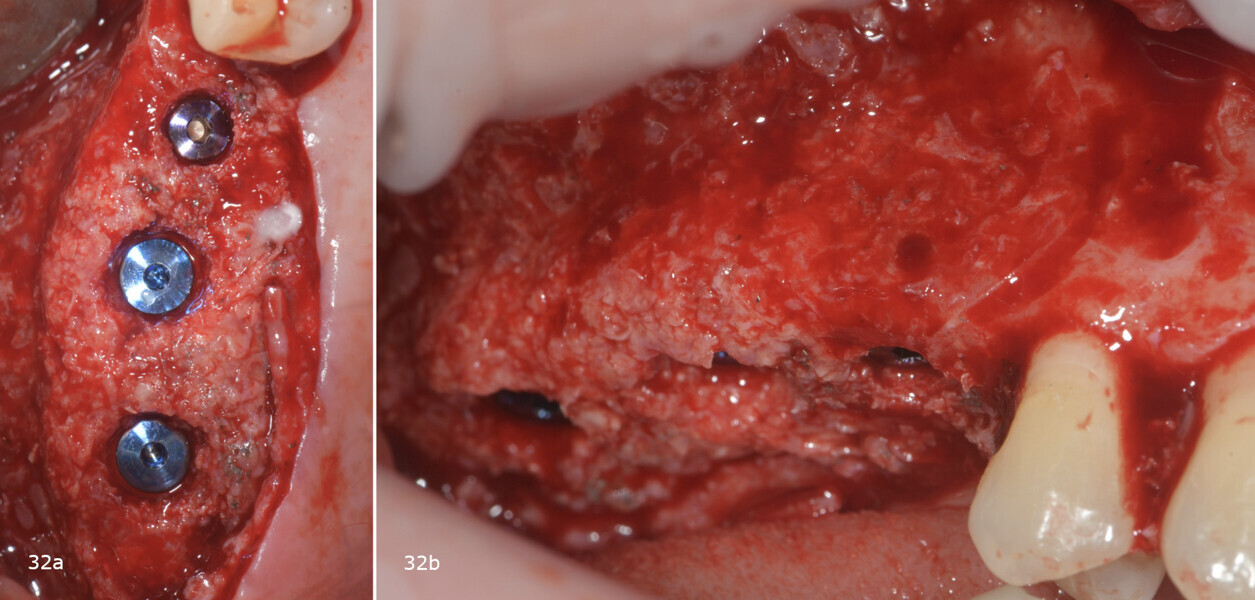
Subsequently, the surgical guide was placed and fixed in the planned position, the implant sites were prepared with progressive dedicated drills and three conical implants (T3, ZimVie) were placed in sites #15, 16 and 17 according to the prosthetically guided plan obtained from the guided surgery software (Figs. 29, 30a-c, 31a & b). The implants were covered to allow for proper osseointegration, and first intention closure was performed (Figs. 32a & b). After implant placement, a dental panoramic tomogram was taken (Fig. 33).
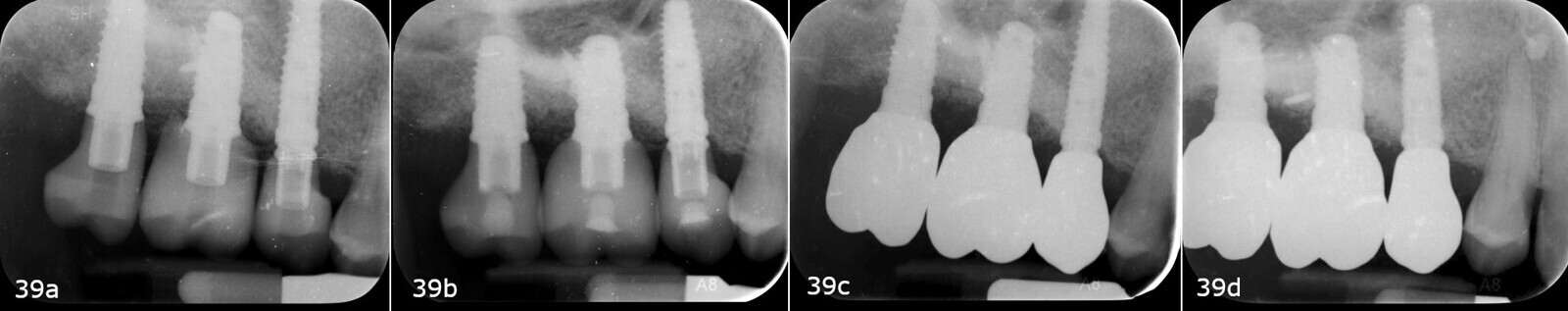
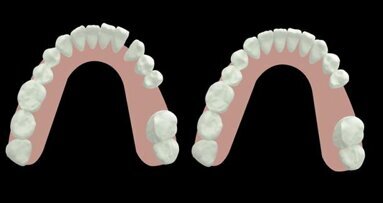
After three months, the implants were exposed through an apically positioned flap to increase the amount of keratinised tissue on the vestibular side of the implants and to realign the mucogingival junction, previously shifted towards the palate. Flared healing screws were placed to promote proper transmucosal healing. After one month, single ceramic crowns were placed for the first functional loading and temporary restoration while waiting for complete bone maturation (Fig. 34). After six months, the crowns were replaced with zirconia crowns for the final functional loading and the definitive restoration (Figs. 35–38). Clinical and radiographic follow-ups at the first functional loading, at six months, 12 months and 24 months showed the health of the peri-implant tissue and the maintenance of peri-implant bone levels (Figs. 39a-d).
Acknowledgements
We would like to extend our deepest gratitude to all the team members involved in the successful completion of this case. Special thanks goes to Cracco Mariano, who meticulously crafted the ceramic crowns used in this case.



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East








































To post a reply please login or register