The following case report describes a successful immediate implant placement in a mandibular first molar position with Straumann TLX and an immediately functional restoration followed up for one year.
Initial situation
A 68-year-old male patient, a non-smoker, presented with controlled Type 2 diabetes. He had undergone previous dental implant treatments with positive results in the past. The patient presented to the office with tooth #36 in a non-restorable condition with indication for extraction. He requested a dental implant as the treatment choice.
Various treatment possibilities were discussed:
- extraction, healing and conventional implant placement;
- extraction and immediate placement with conventional healing and then a definitive prosthesis; or
- extraction, implant placement and immediate functional loading of the implant.
In his previous treatments, the patient had experienced successful treatment outcomes with the one-tooth, one-time technique, which is a technique that provides the definitive crown to be produced and seated in immediate occlusal function right after the surgical procedure. For this particular case, given the systemic condition, it was suggested that a crown made of temporary material be put into immediate function during the healing phase to ensure that the systemic condition would not affect the soft-tissue healing and contours before starting the definitive crown. After full discussion, the patient opted for the third solution. All the parameters supported the chosen treatment.
Treatment planning
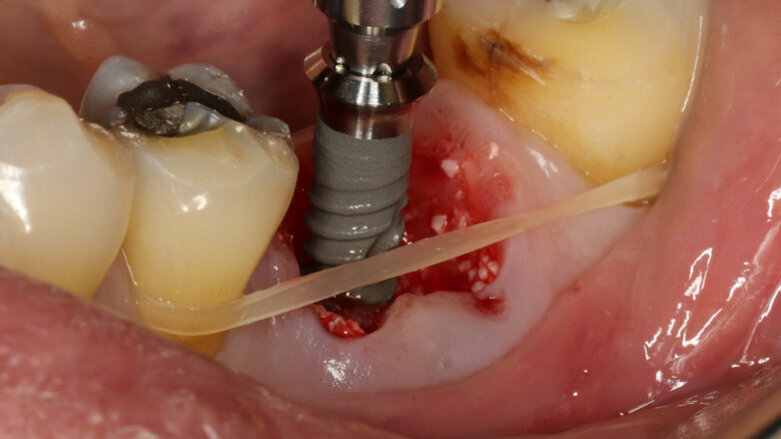
After careful assessment of the patient’s anatomical condition through a panoramic radiograph and CBCT scan (Figs. 1–3), it was possible to verify ideal interradicular bone availability, allowing the following treatment plan:
- minimally traumatic tooth extraction;
- immediate implant placement (Straumann TLX, 3.75 × 12.00 mm);
- intra-oral scanning;
- temporary crown design and chairside milling;
- immediate provisional crown in function; and
- after osseointegration and soft-tissue maturation, proceeding with the definitive crown.
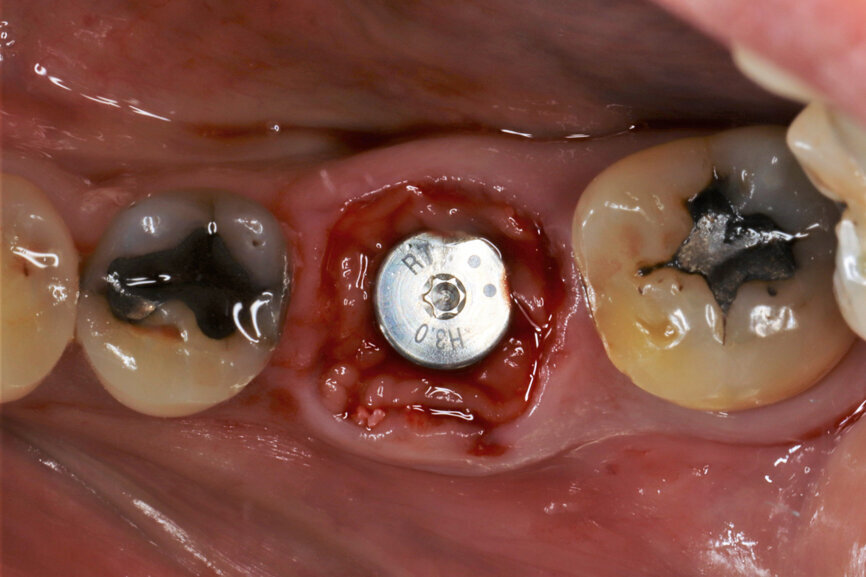
Fig. 1: Intra-oral occlusal view.
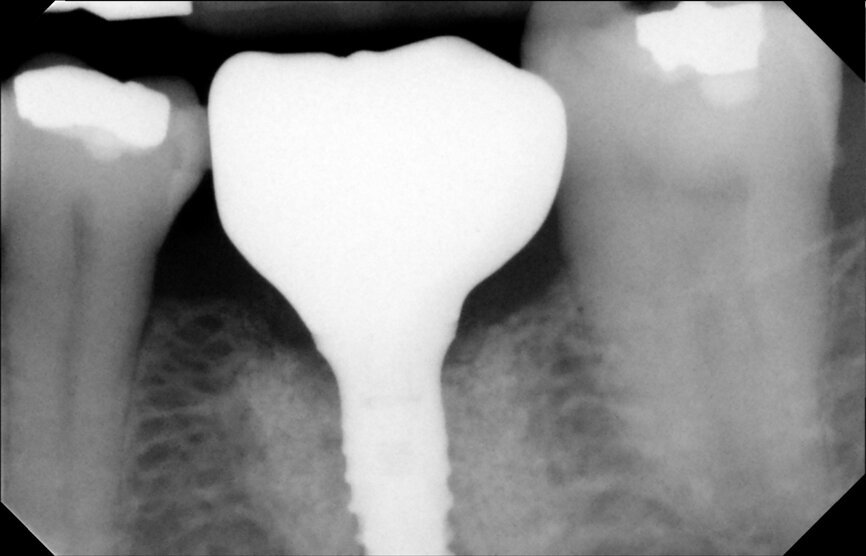
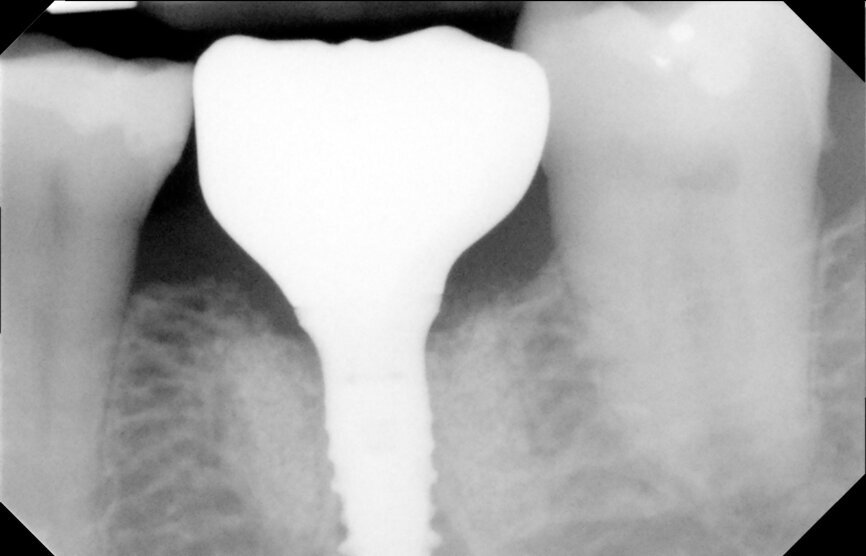
Fig. 2: Panoramic radiograph.
Fig. 3: Tooth #36 initial situation.
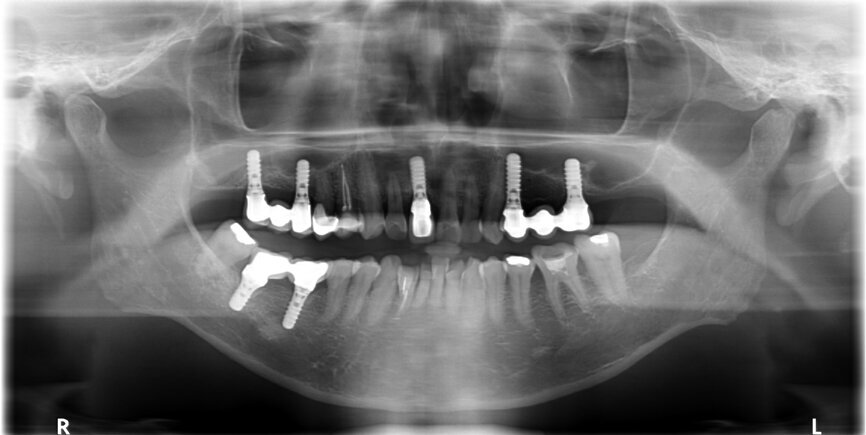
Fig. 4: Root splitting for minimally traumatic extraction.
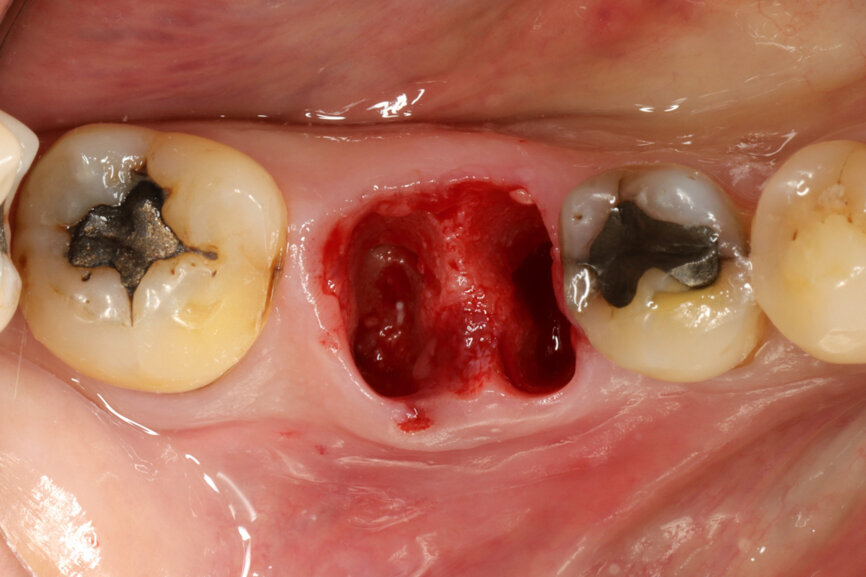
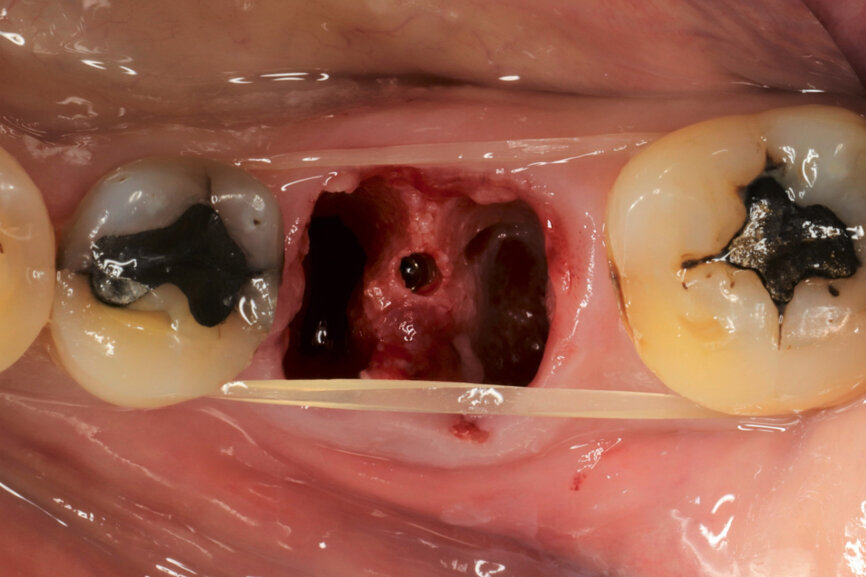
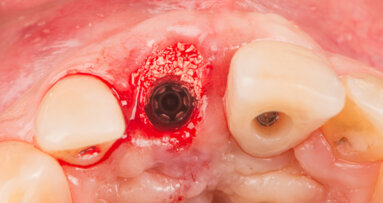
Fig. 5: Socket dimensions preserved.
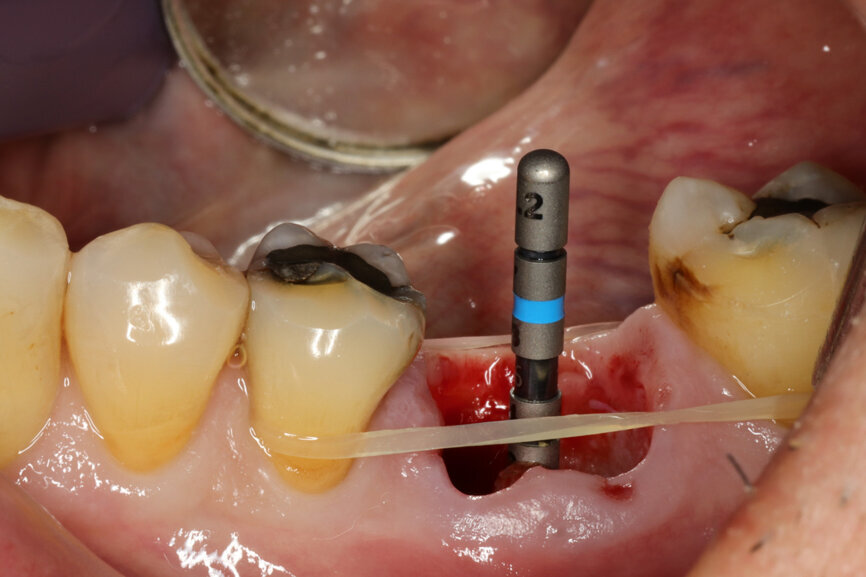
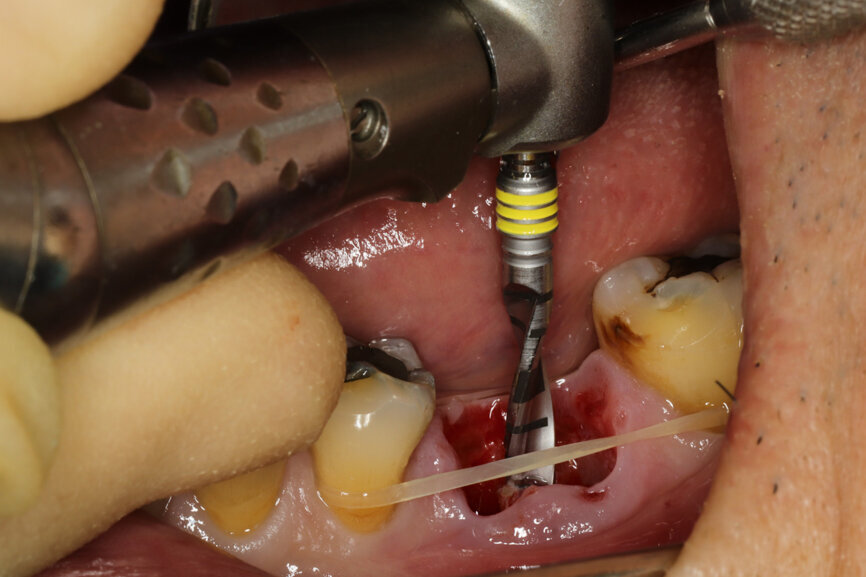
Fig. 6: Osteotomy with the ⌀ 2.2 mm drill.
Fig. 7: Centrally oriented osteotomy.
Fig. 8: Alignment of the ⌀ 2.2 mm drill, confirming 3D position.
Fig. 9: Alignment of the ⌀ 2.2 mm drill, confirming 3D position.
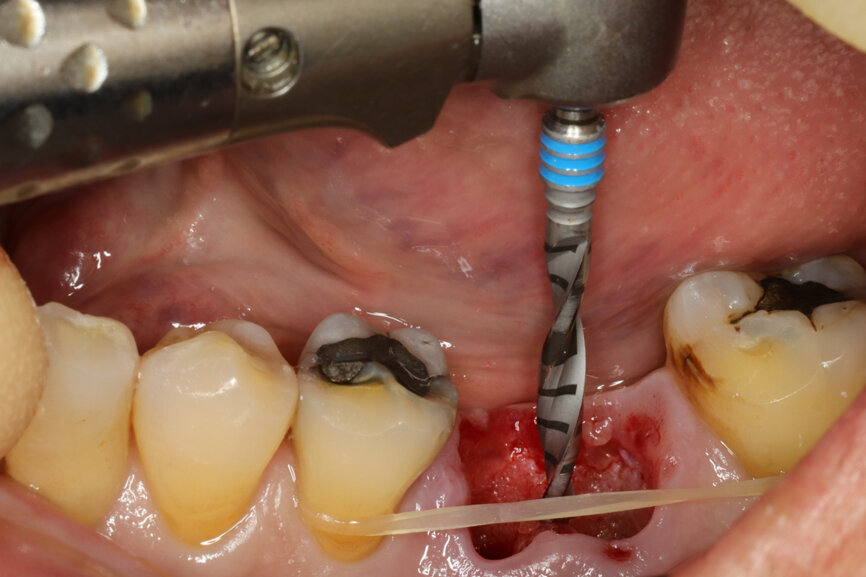
Fig. 10: Osteotomy with the ⌀ 2.8 mm drill.
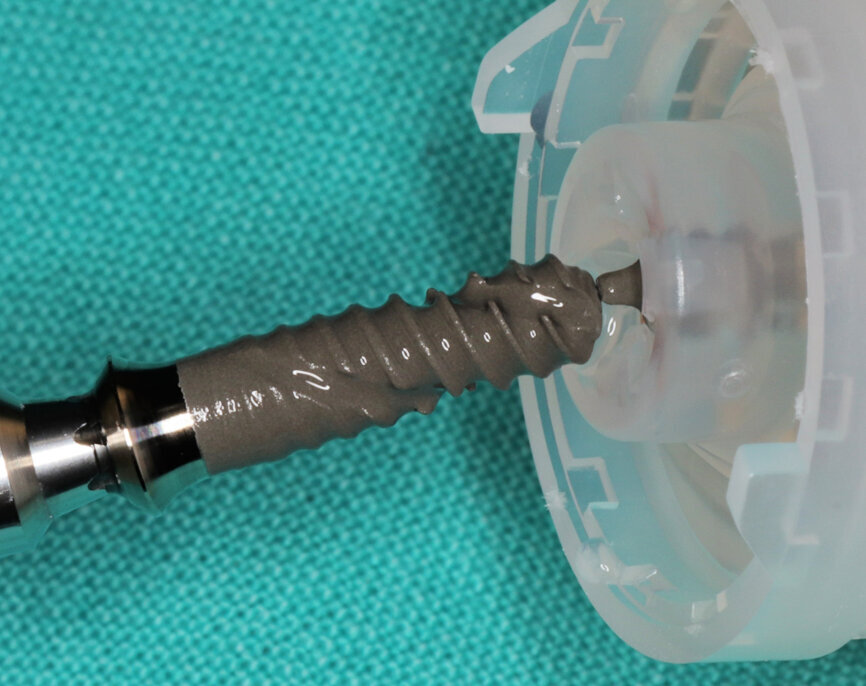
Fig. 11: Straumann TLX implant ready for pick-up on the vial cap.
Fig. 12: Direct implant pick-up with insertion driver.
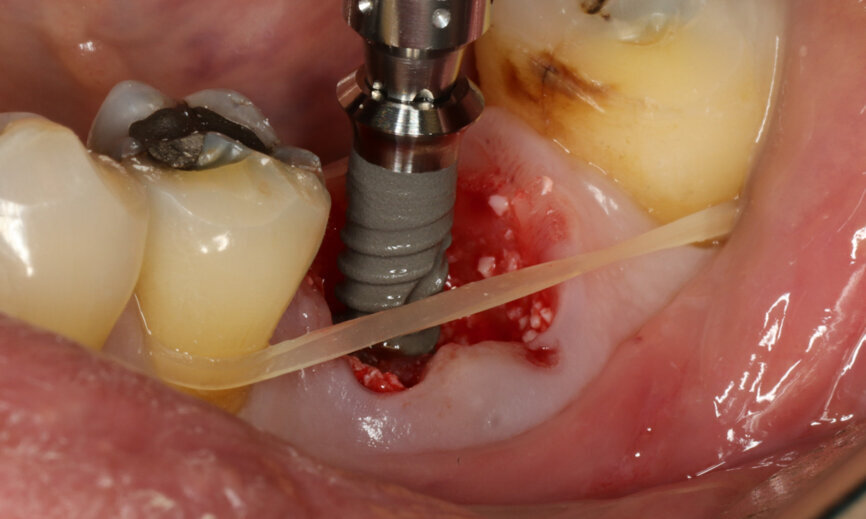
Fig. 13: Straumann TLX implant insertion.
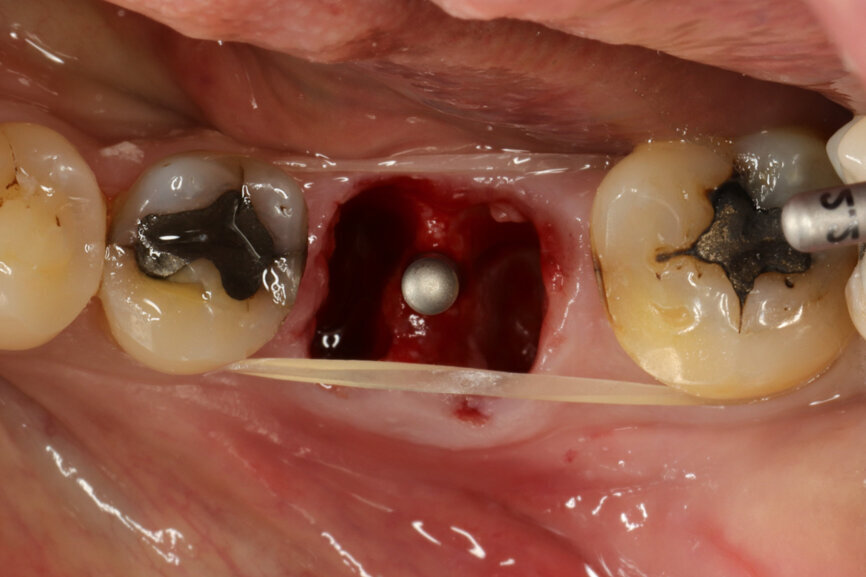
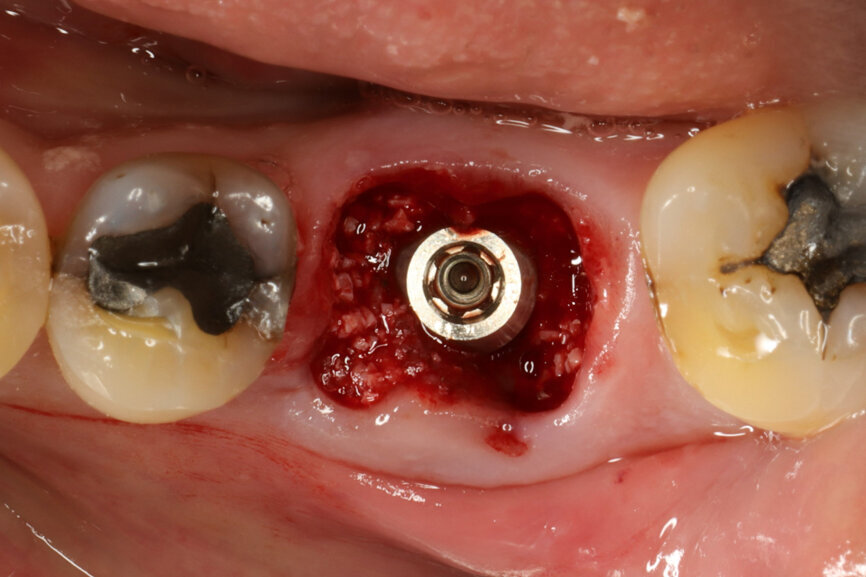
Fig. 14: Implant in final position with bone augmentation.
Fig. 15: Implant in final position with A-PRF protecting the bone substitute granules.
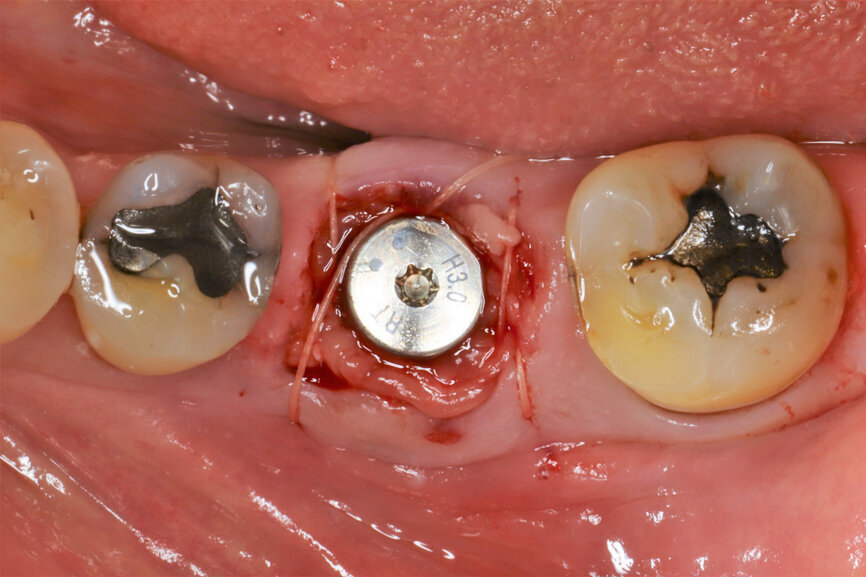
Fig. 16: Sutures to stabilise the biomaterials in place.
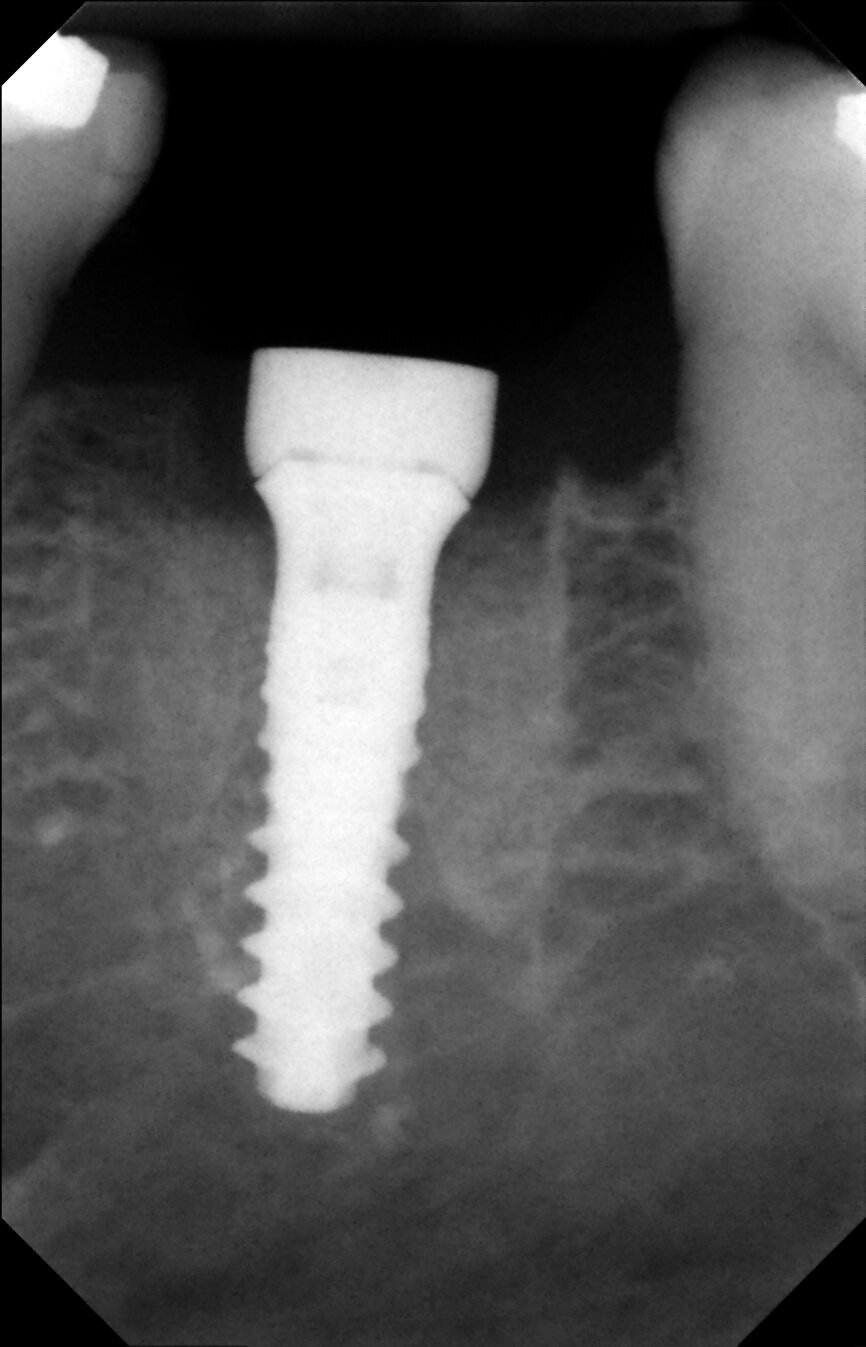
Fig. 17: Periapical radiograph after implant placement.
Fig. 18: Temporary crown.
Fig. 19: Temporary crown immediately seated.
Fig. 20: Temporary crown immediately seated.
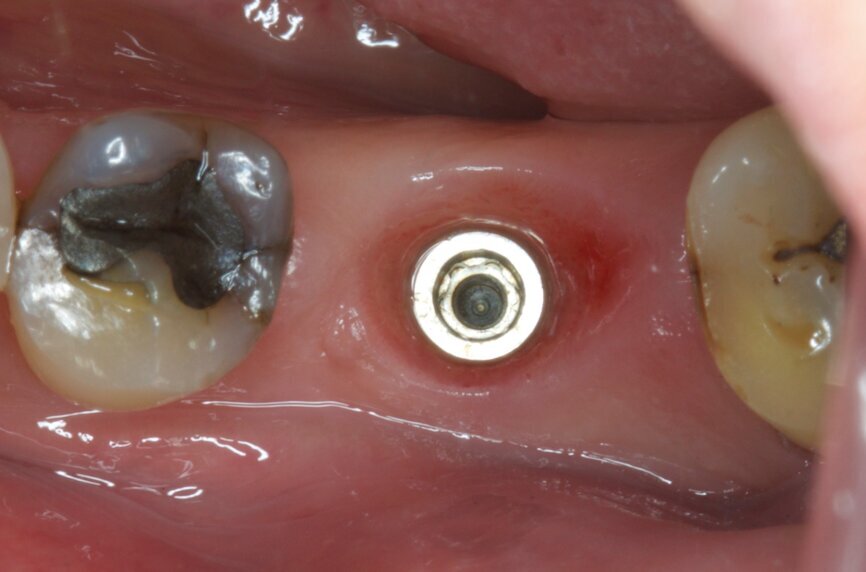
Fig. 21: Gingival healing ready for initiation of definitive crown.
Fig. 22: Scan body in position for digital impression.
Fig. 23: Temporary crown removed and monolithic zirconia crown ready for insertion.
Fig. 24: Final result—lateral view.
Fig. 25: Final result—occlusal view.
Fig. 26: Final outcome radiograph.
Fig. 27: Straumann TLX one-year follow-up clinical outcome.
Fig. 28: Straumann TLX one-year follow-up clinical outcome.
Fig. 29: One-year follow-up radiograph showed peri-implant stability.
Surgical procedure
The surgical procedure was carried out under conscious sedation with local anaesthetic, and routine sterile preparations for surgical procedures were followed. To preserve the gingival and surrounding walls as far as possible, a flapless minimally traumatic approach to the extraction was employed by splitting the roots in different directions (Fig. 4). Extra precautions were taken not to inflict any trauma, not even by the suction device on the papilla and any surrounding soft tissue. A simple orthodontic elastic was placed around the adjacent teeth to delimitate the buccal and lingual red zone margins that should not be encroached upon.
It was possible to verify solid interradicular bone availability (Fig. 5), extending further the limits of the root apices and allowing for a centrally oriented osteotomy. The implant bed preparation started with the use of a needle drill at 800 rpm, followed by the ⌀ 2.2 mm and ⌀ 2.8 mm drills (Figs. 6–10). The implant was placed with the use of ratchet and torque control, reaching the desired final position at a 50 N cm torque value (Figs. 11–13). The socket was then augmented with bovine-derived bone substitute impregnated with advanced platelet-rich fibrin (A-PRF) and finalised with sutures to keep the A-PRF application immobile, and a 3 mm healing abutment was placed (Figs. 14–17).
The patient also received an intra-operative antibiotic with 4 mg dexamethasone intravenously and received standard postoperative care with analgesics, chlorhexidine mouthwash and antibiotic for five days.
Prosthetic procedure
The patient was sent to the prosthodontist, and the immediate restoration technical work followed a digital workflow that included an intra-oral scanner (TRIOS Pod, 3Shape) and CAD/CAM processing using Straumann CARES Digital Solutions (Dental Wings). A PMMA crown was milled and cemented to a prefabricated titanium abutment (Variobase, Straumann; Fig. 18). A few hours later, the patient left the office having received an immediate implant and a functional provisional screw-retained restoration (Fig. 19 & 20).
In Taiwan to celebrate the Chinese New Year, the patient was caught up in the first COVID-19 restrictions, and his return to the office was compromised for a few days.
Upon the patient’s return, the definitive crown placement was initiated by another intra-oral scan to copy all the gingival contours after healing (Figs. 21 & 22). A full monolithic zirconia crown was milled and cemented to a Variobase abutment (diameter: 5 mm; height: 6 mm) and properly seated, occlusal and contact points checked. The screw access hole was properly closed with PTFE tape and light-polymerised composite (Fig. 23).
Treatment outcomes
From a clinical perspective, the immediate placement and function were very well indicated as they could be verified through the gingival margins and health, and bone levels throughout the healing phase, and final and one-year follow-up images (Figs. 24–29).
The patient was very satisfied with the result in relation to masticatory performance and aesthetics. In addition, given the time restrictions to undergoing several treatment appointments, the possibility of having a very close to final restoration immediately after the surgical procedure requiring only another session to finalise the treatment was, according to him, far more desirable than his earlier dental implant procedures.
Immediate implant placement and loading have become increasingly prevalent in modern dentistry, especially in the aesthetic zone, where patients typically ...
Placing an implant immediately after tooth extraction offers several advantages, including a reduced treatment time, fewer surgical sessions, possibility of...
Many factors can be related to apical root resorption and rounding, among them orthodontic movement and occlusal trauma. In severe cases, the tooth can even...
BASEL, Switzerland: Straumann is pleased to report the very positive results of the first human case study to track the condition and progress of a patient ...
Thanks to the very high accuracy of modern intra-oral scanners, excellent design software and reliable production systems, restoring an implant with a ...
Straumann Campus provides dental professionals with a myriad of webinars with a focus on implant dentistry and orthodontics. In the coming weeks, the online...
BASEL, Switzerland: With implant dentistry continually developing and evolving, so too are some of the low-cost options. In a recent move to secure a larger...
BASEL, Switzerland: Straumann fully launched its TLX implant system at the International Team for Implantology (ITI) World Symposium 202ONE, which is the ...
BASEL, Switzerland: Continuing on from a strong 2017, the Straumann Group has reported a positive start to the first quarter of 2018. With double-digit ...
Live webinar
Thu. 26 March 2026
12:30 pm EST (New York)
Dr. Laurence Adriaens, Dr. Ghida Lawand BDS, MSc
Live webinar
Mon. 13 April 2026
1:00 pm EST (New York)
Dr. David Norré, Dr. Tommie Van de Velde DDS, MSc, PhD
Dr. Piet Haers Oral and Maxillofacial Surgeon



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East
























































To post a reply please login or register