Discussion
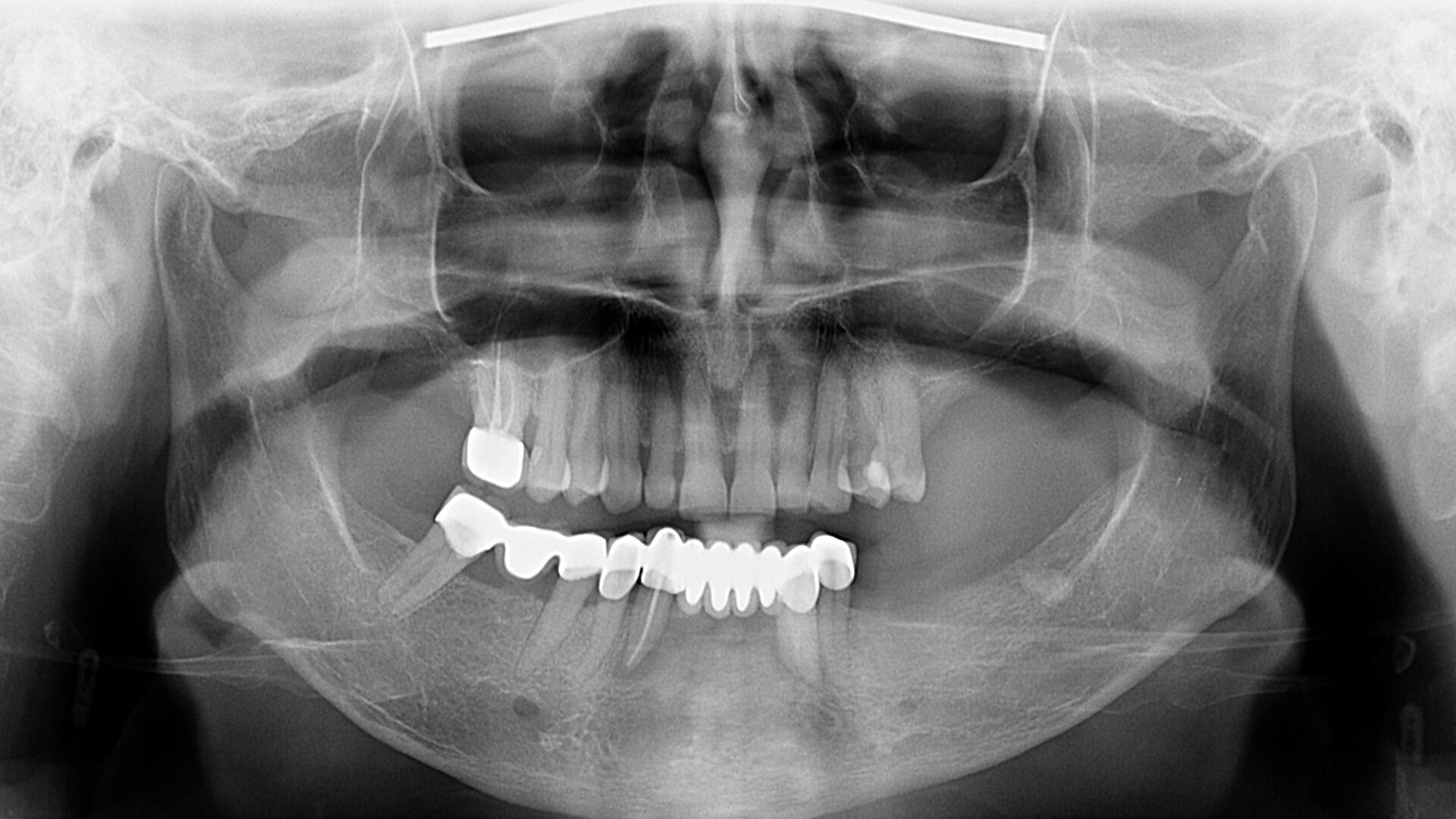
A notable consideration in this case was the clinically healthy and asymptomatic condition of the temporomandibular joints. While centric relation is commonly preferred in full-mouth rehabilitation owing to its reproducibility and stability, maintaining maximal intercuspal position was chosen in this case. This decision was based on the absence of maxillary restoration and the patient’s asymptomatic temporomandibular joints. Avoiding unnecessary alteration to the patient’s habitual occlusion provided easier adaptation and comfort, aligning clinical prosthodontic principles with patient-specific conditions and preferences.10, 11
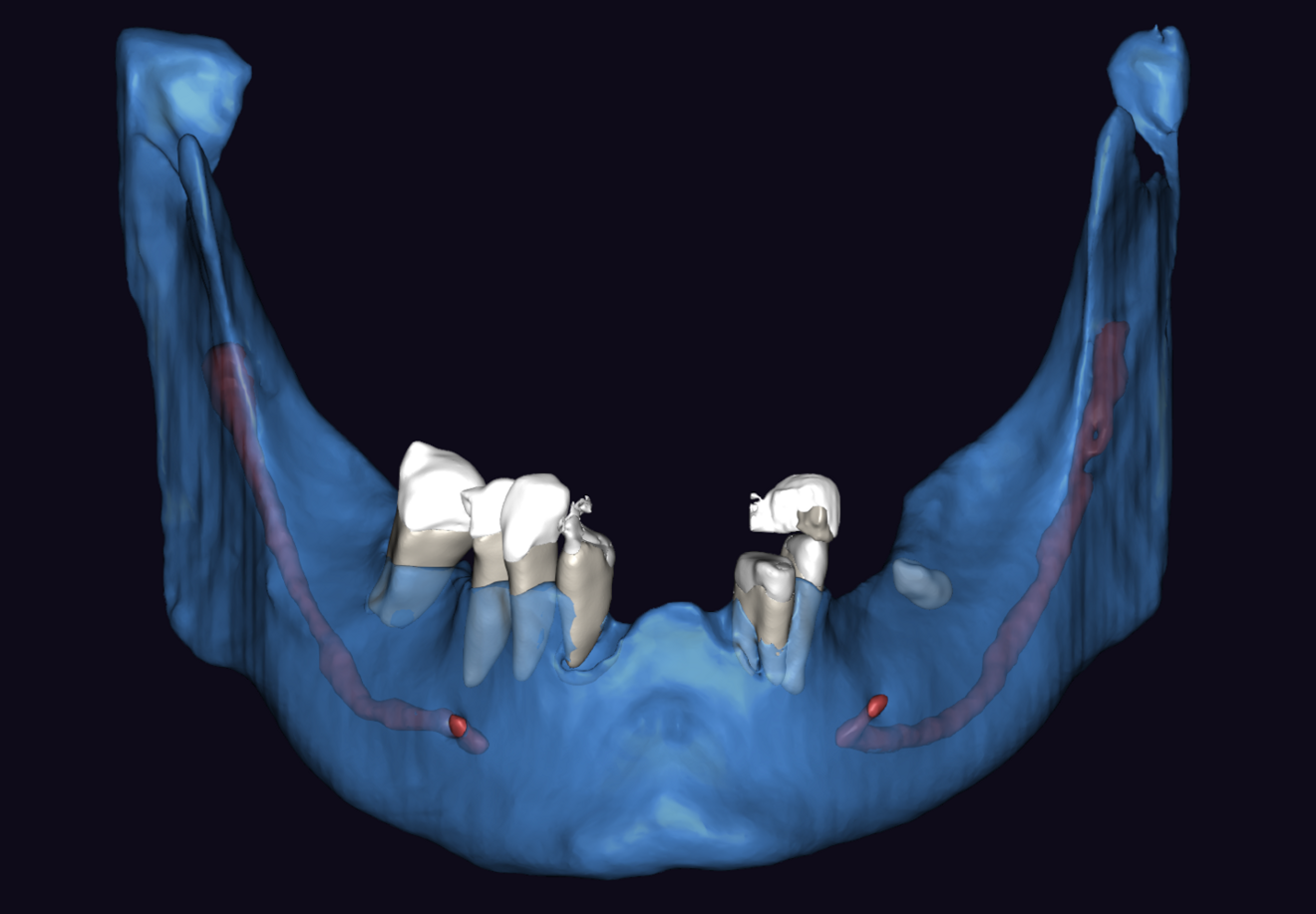
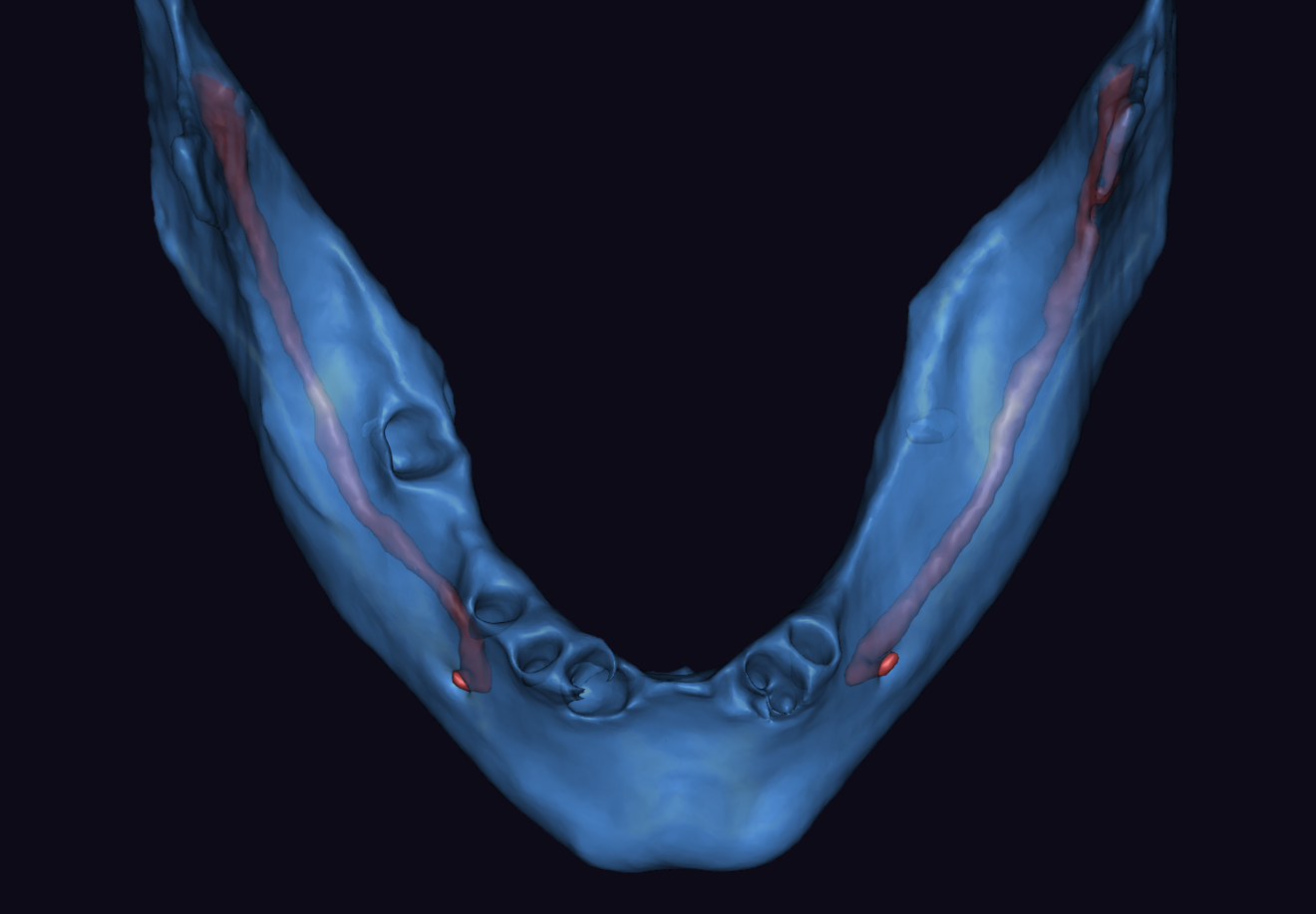
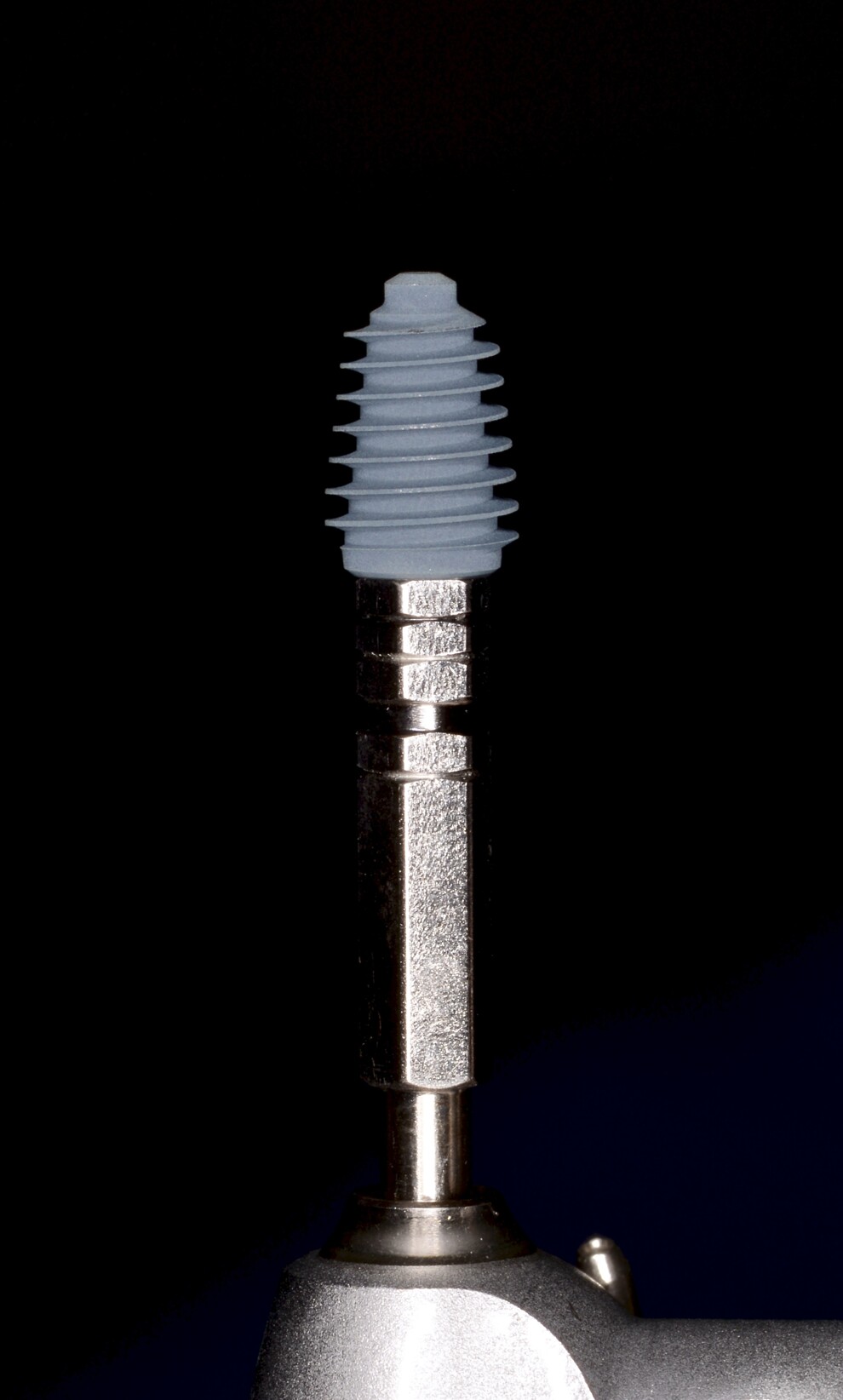
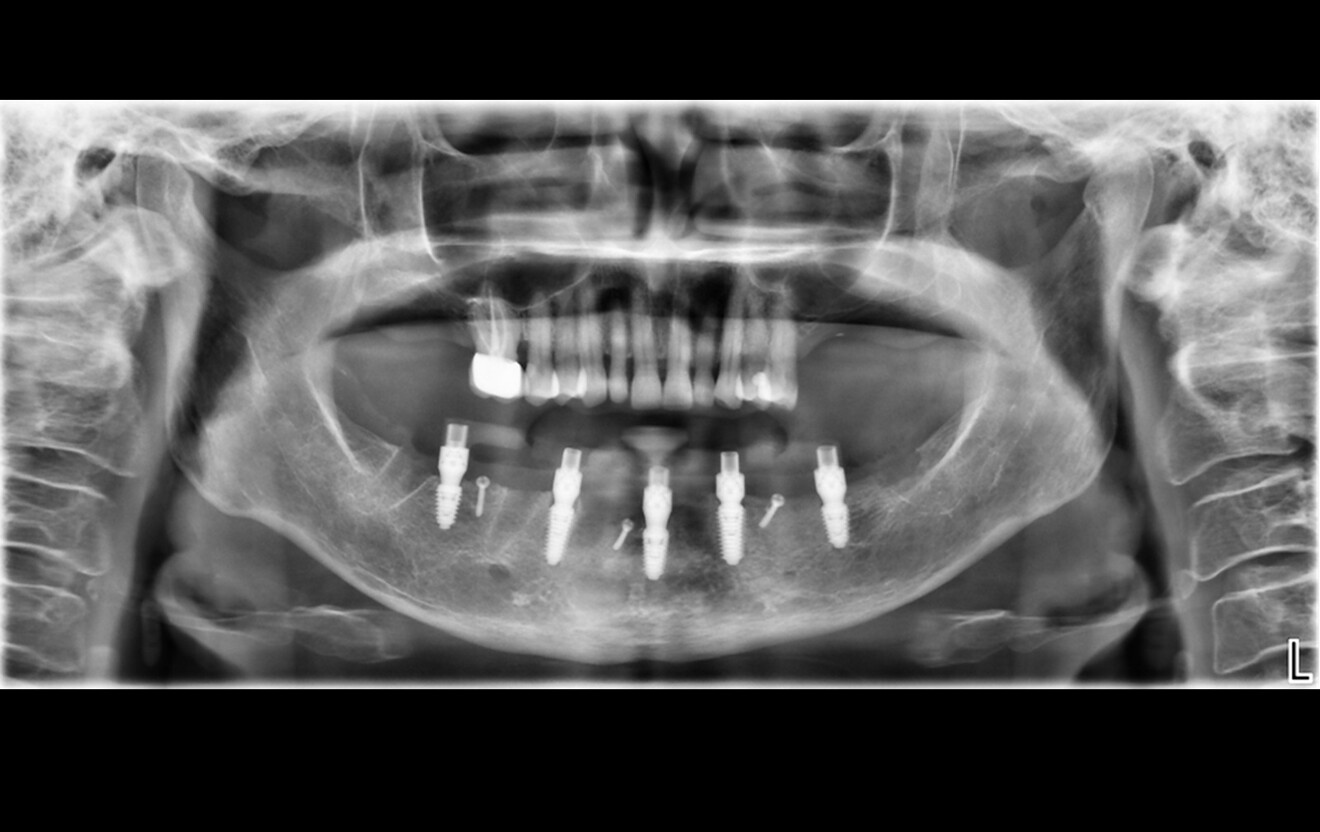
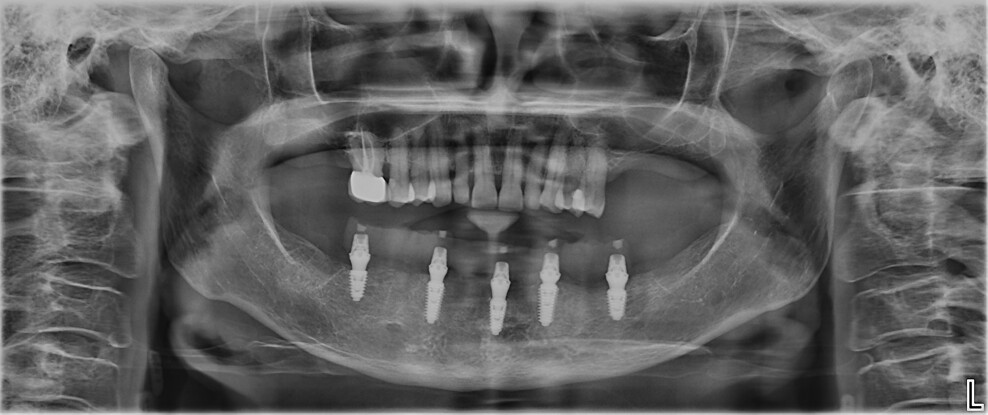
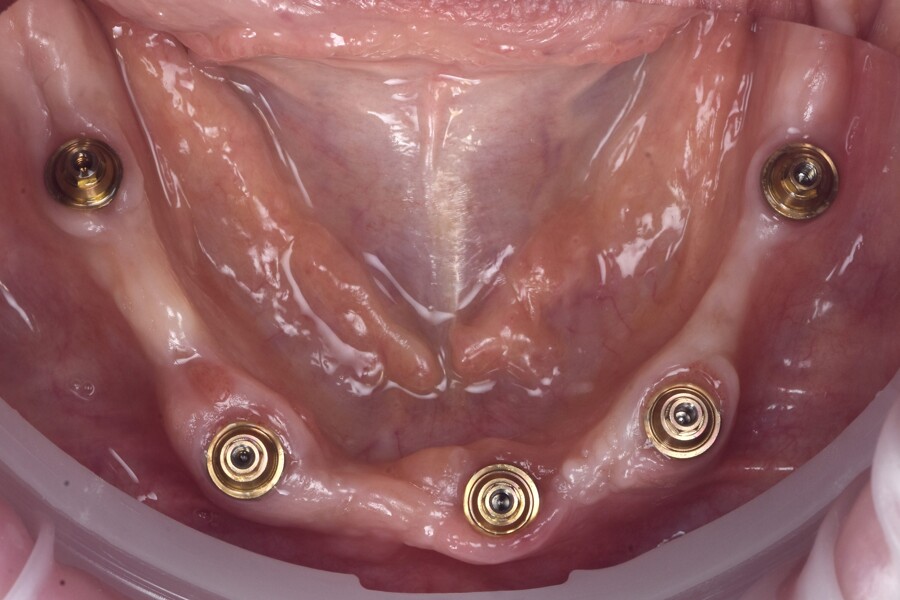
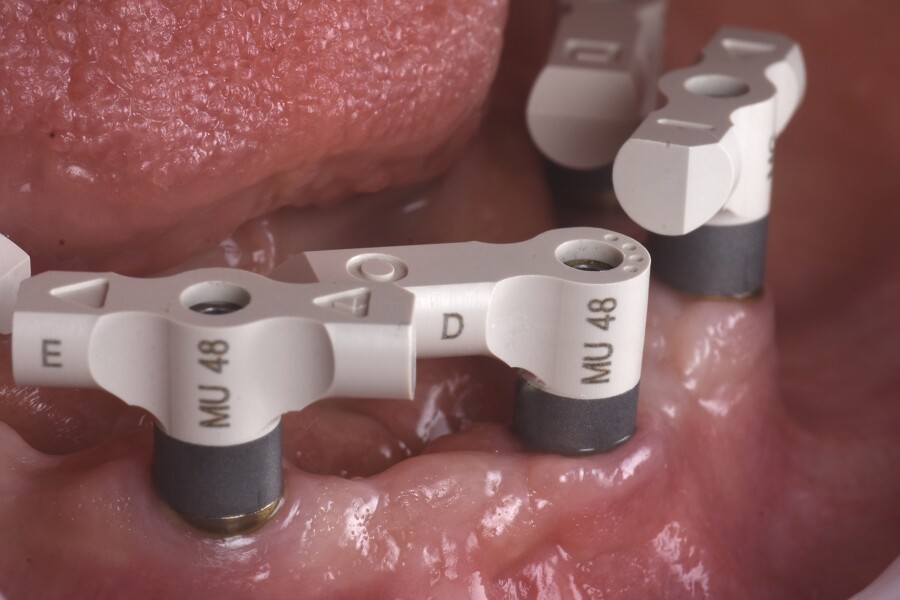
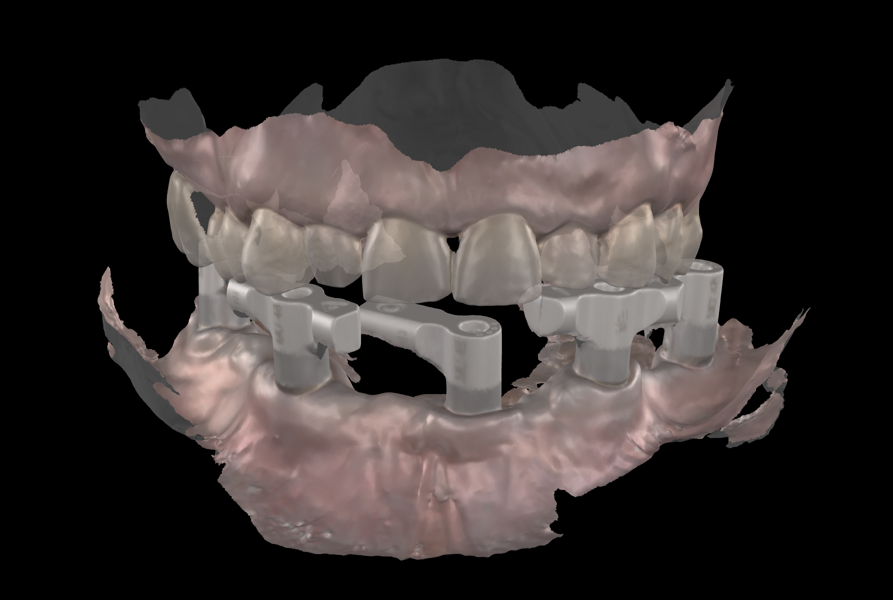
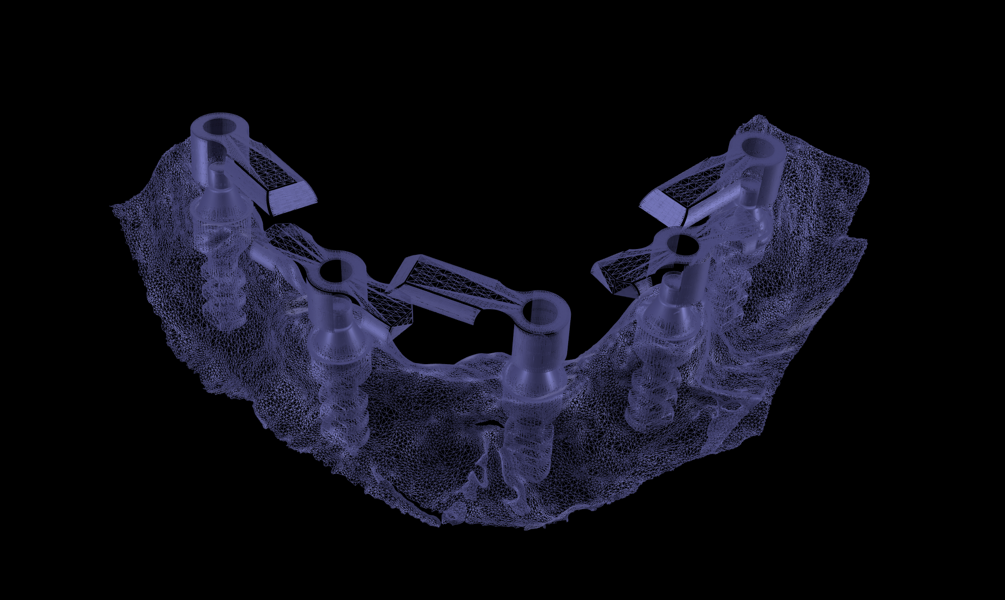
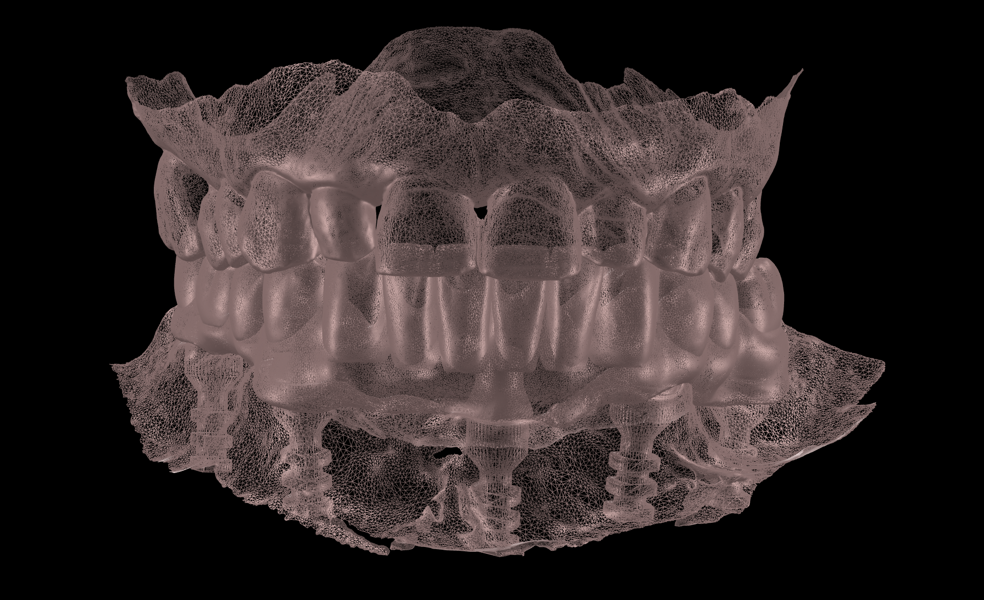
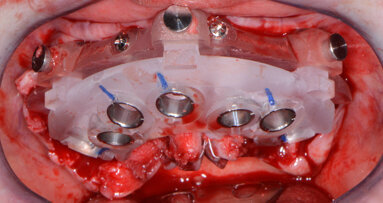
Another aspect worth highlighting is the decision to perform the prosthetic workflow entirely at the abutment level. This approach aligns with the one abutment, one time concept, avoiding repeated implant–abutment disconnections and minimising the disruption of hemidesmosomal attachment. The multi-unit platform facilitates prosthetic passivity, because implant angulations are less critical when using multi-unit abutments. Higher angulation differences can be compensated for with angled multi-unit abutment as well. The multi-unit platform is designed for ease of use, simplifying scanning, impression taking, try-in and final delivery. It also allows the prosthetic platform to sit more coronally, facilitating easier access for evaluation of fit and passivity. For this particular implant system, implant-level restorations are contra-indicated owing to the Morse taper connection, which makes it challenging to seat multi-implant prostheses passively when axes diverge. Thus, an abutment-level workflow provides mechanical, biological and practical advantages in full-arch rehabilitation.
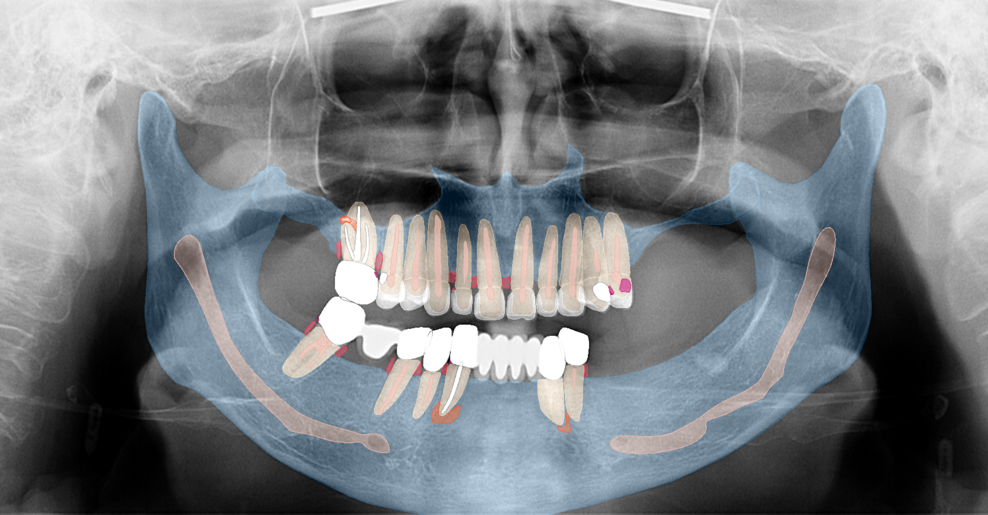
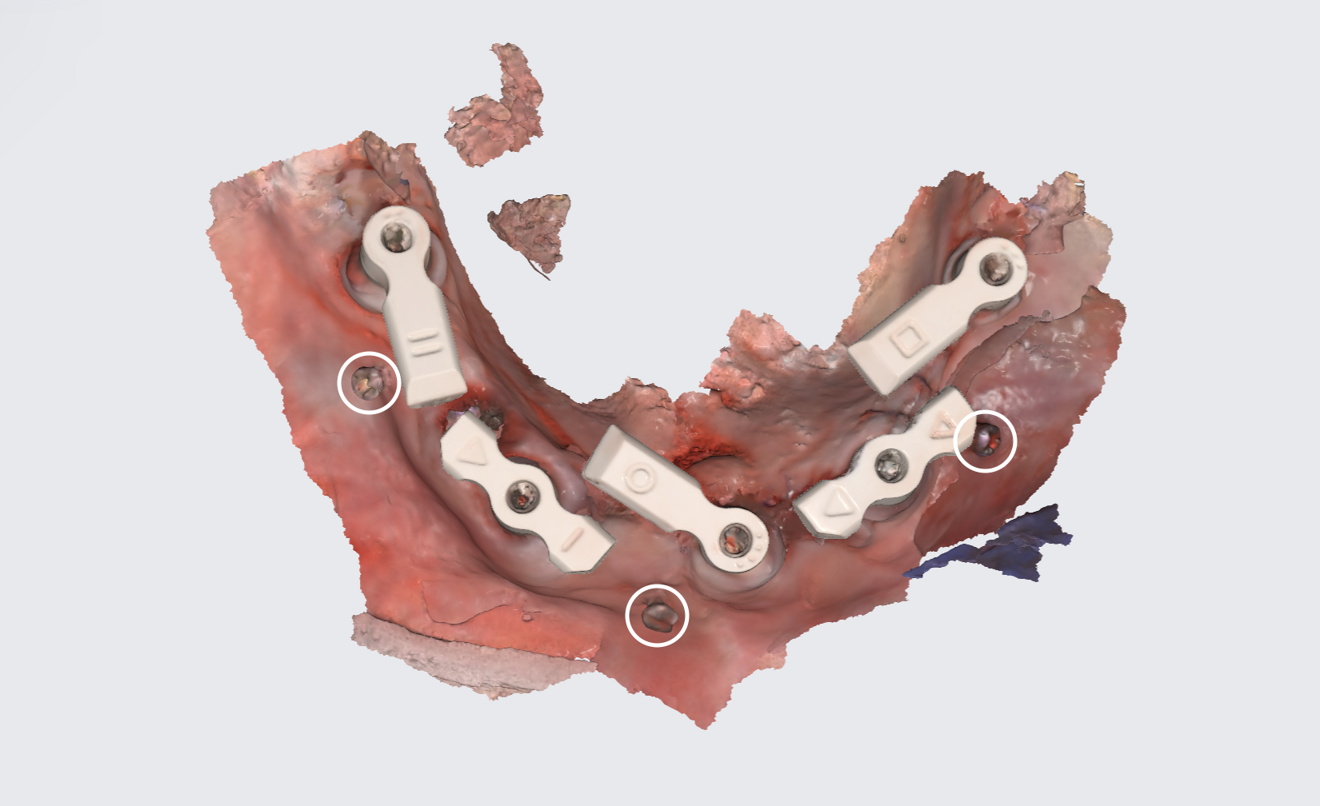
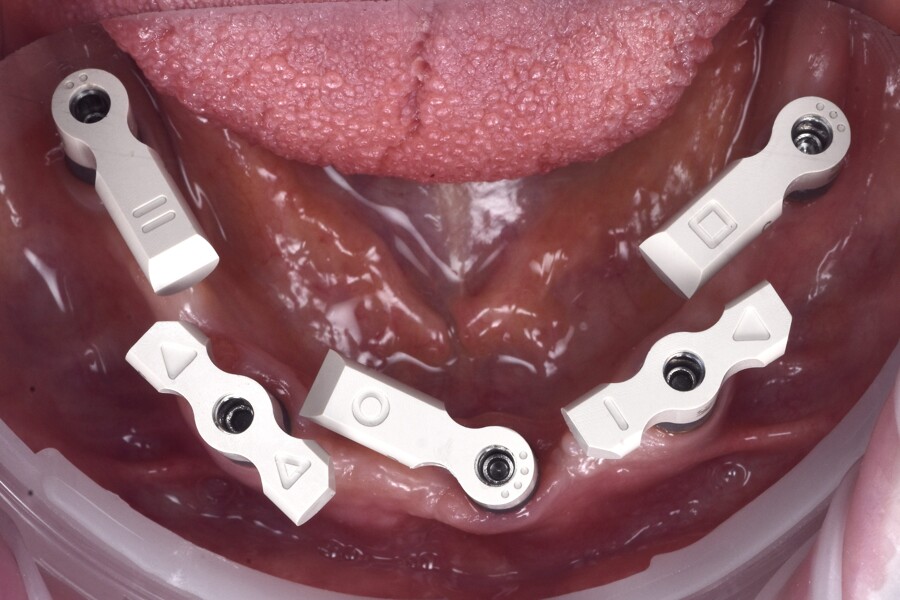
The use of fiducial markers in this case also deserves mention. While alternatives such as adhesive markers or digitally designed tissue trackers have been described, the principle remains the same: stable, scanner-visible reference structures should be placed before surgery that remain unchanged throughout the procedure. This ensures easily identifiable landmarks for aligning preoperative and postoperative data, improving the accuracy of digital workflows in full-arch cases.
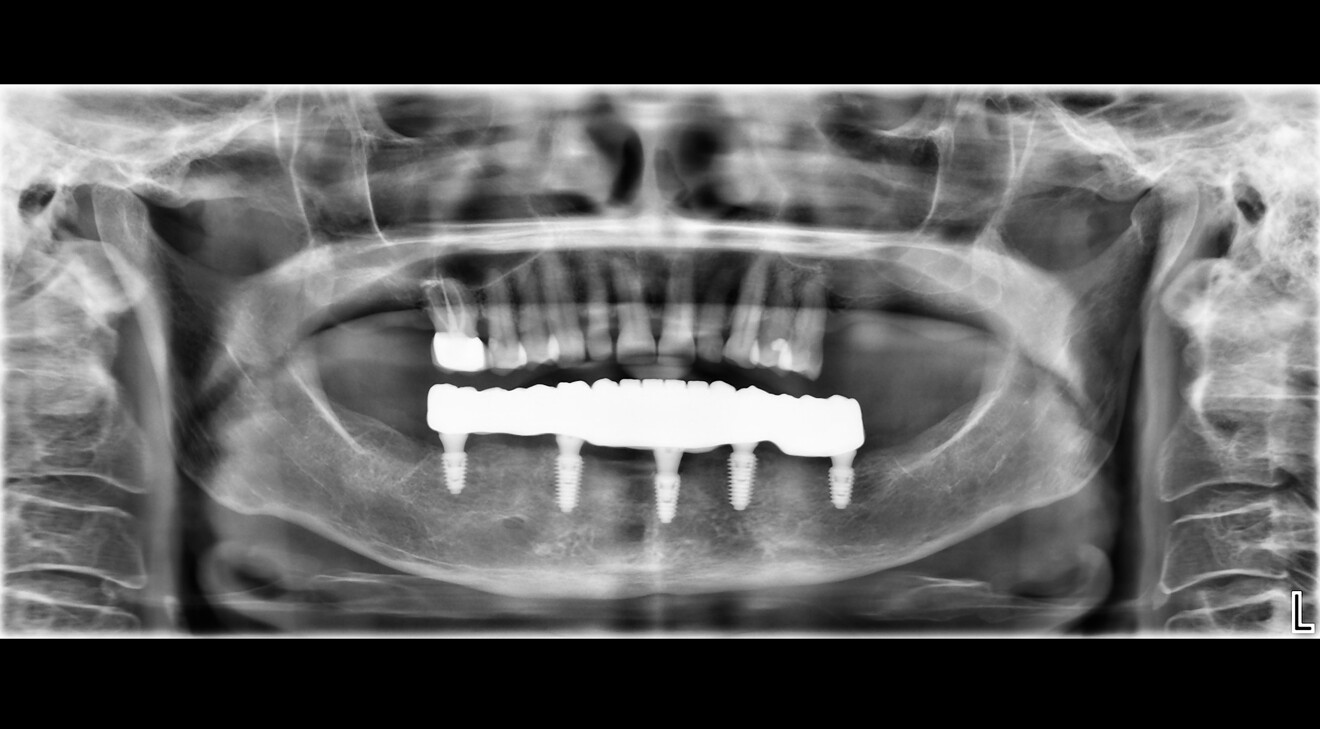
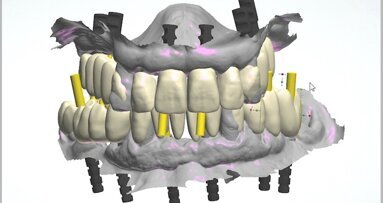
The material selection in this case was also a key consideration. A titanium bar supporting a monolithic zirconia superstructure was chosen over a full-zirconia or metal–ceramic restoration. This approach combined strength, aesthetics and long-term reliability. While full-zirconia restorations are becoming increasingly popular for their aesthetic qualities and structural durability as monolithic restorations, they are prone to fracture if passive fit is compromised, particularly in the mandible owing to its inherent flexure. Conversely, metal–ceramic restorations, while robust, lack the same level of translucency and natural aesthetics and are not suitable for a fully digital workflow, although the framework could be used in the CAD/CAM digital workflow. The titanium bar provided a strong, stable framework, while the zirconia superstructure offered superior aesthetics and biocompatibility. This combination represents a balanced solution tailored to the clinical demands and patient expectations of full-arch rehabilitation.
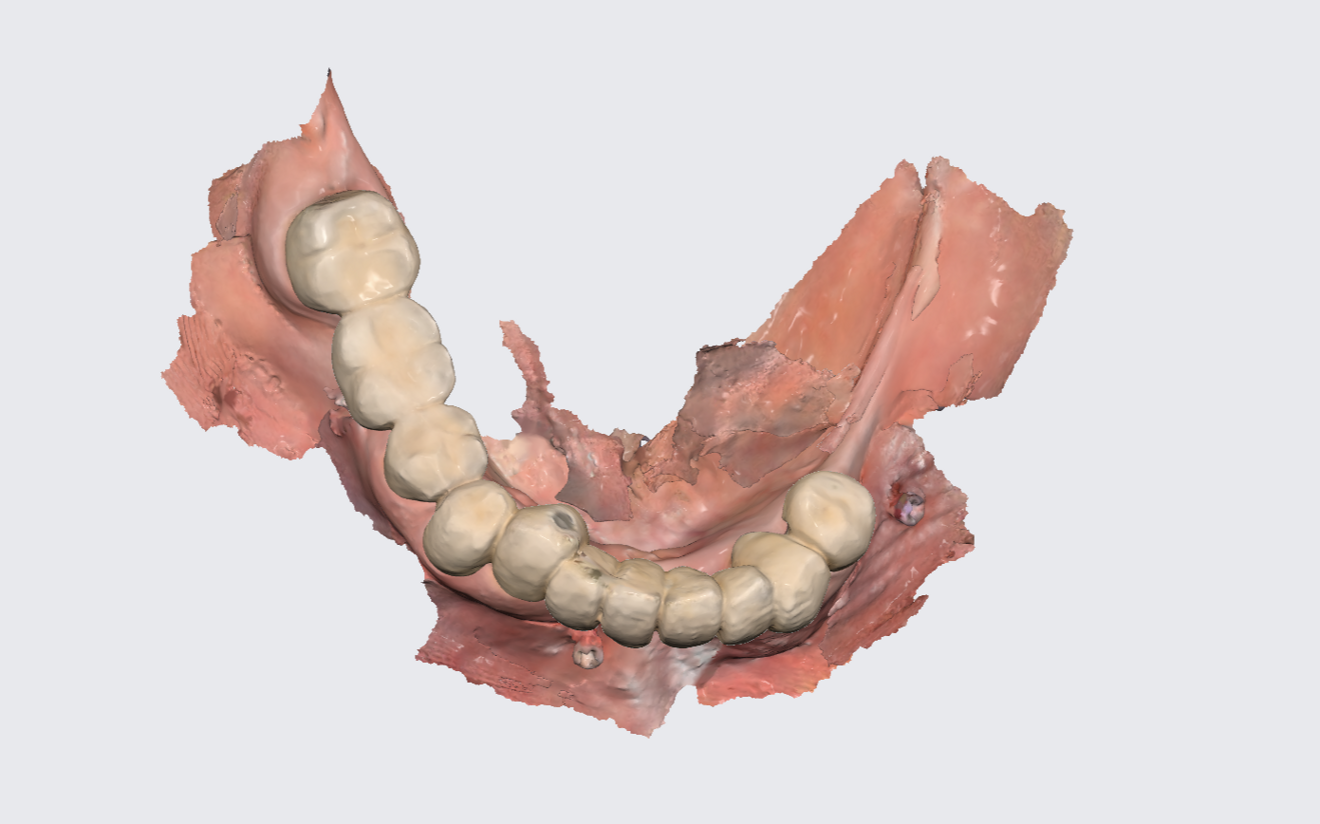
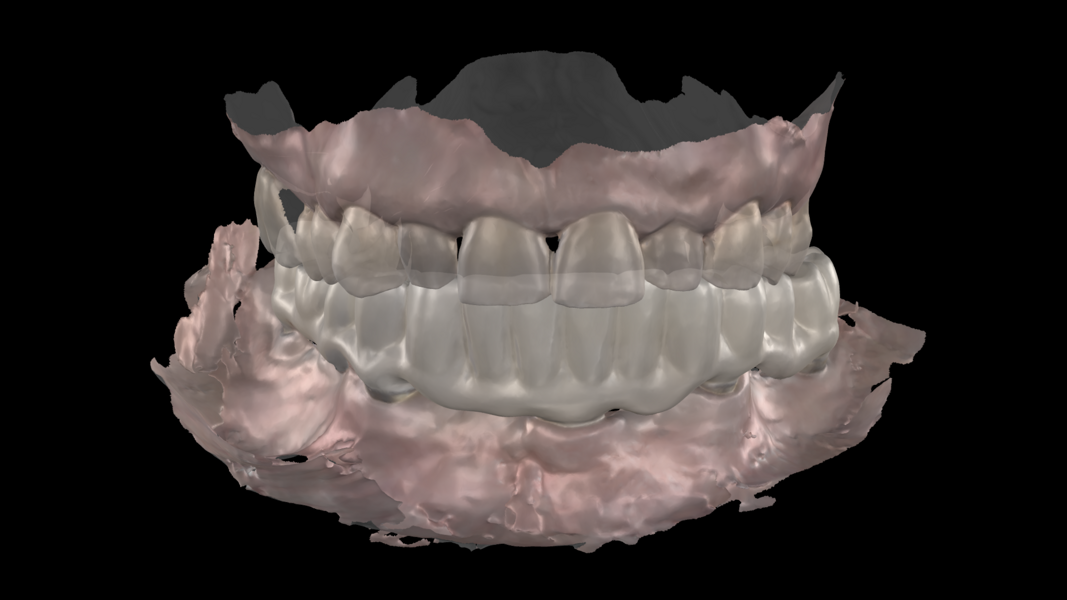
This case demonstrates the importance of a carefully planned, fully digital workflow in full-arch mandibular rehabilitation. Beyond accuracy and predictable fit, the fully digital approach offers increased efficiency, fewer clinical sessions and improved patient comfort compared with conventional impressions. The ability to replicate the provisional restoration’s occlusion and use its design—so-called copy–paste dentistry—further simplifies and streamlines the process.12 Digital workflows also contribute to improved communication between the clinical and laboratory teams and allow for earlier patient function and satisfaction. Importantly, the workflow followed in this case shows that modern digital techniques can deliver outcomes comparable to those of traditional methods and offer added benefits in workflow speed and convenience. Fully digital workflows of this kind highlight the clinical value of the approach.
Conclusion
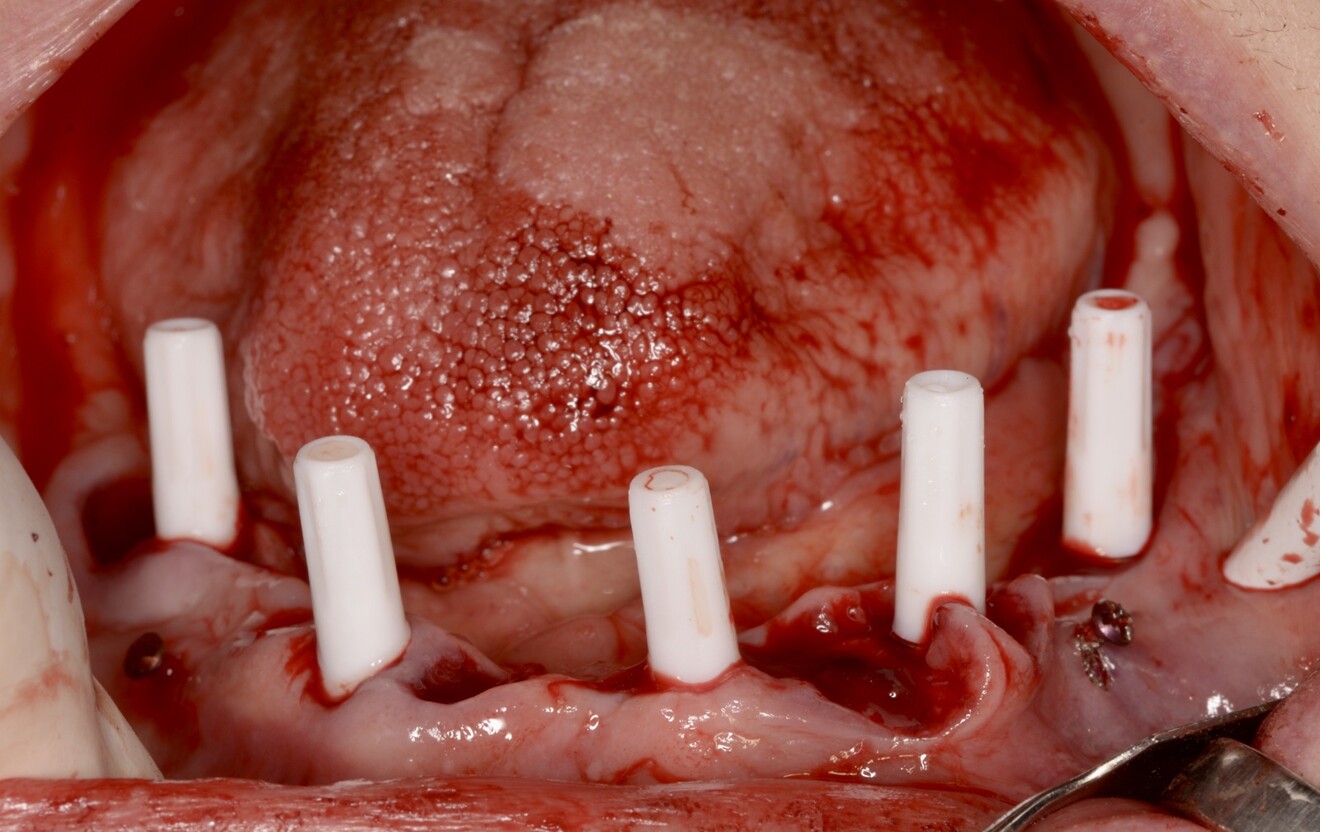
This case demonstrates how a fully digital workflow can facilitate a predictable, patient-centred full-arch rehabilitation in the mandible, even when tooth-preserving treatment is declined. Careful planning, the use of fiducial markers and SmartFlag scan bodies, and adherence to prosthetic principles allowed the team to achieve a passive, functional and aesthetic restoration. Digital workflows offer promising alternatives to conventional techniques, provided their limitations are understood and mitigated.



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East












































To post a reply please login or register