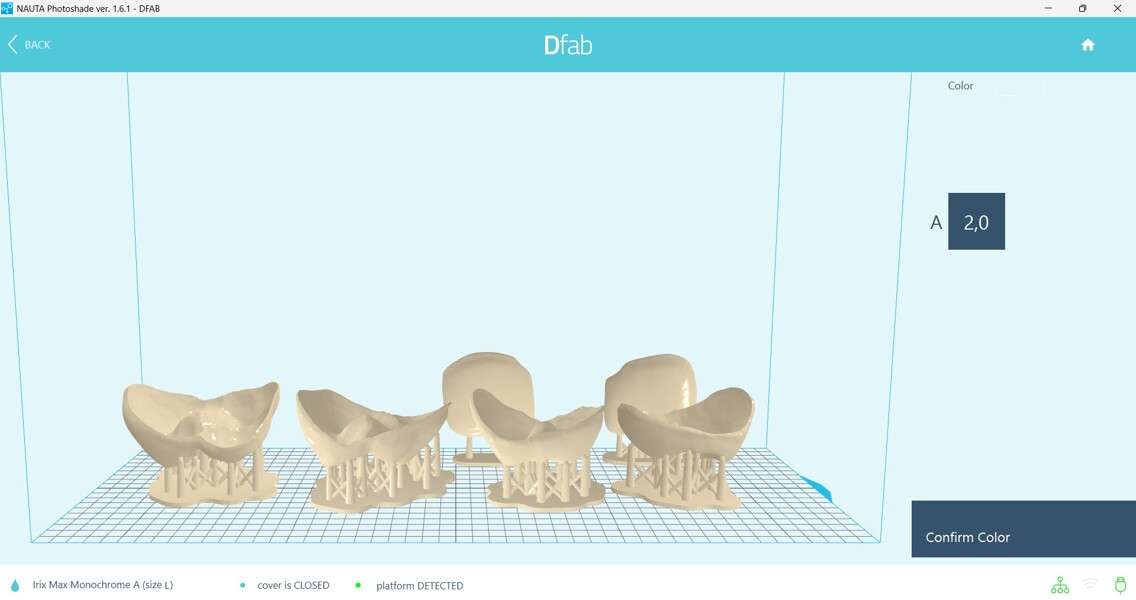
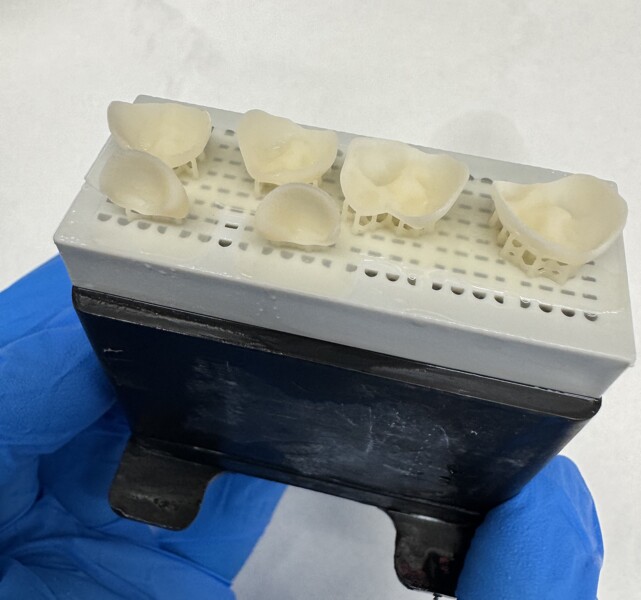
Occlusal elevation was essential to address the deep overbite with mucosal impingement, and the restorations were delivered using a simplified cementation protocol optimised for paediatric patients. A dual-polymerising resin cement and corresponding adhesive system were selected for their ease of use, effectiveness and reduced procedural steps, critical factors in managing treatment within the behavioural limits of very young children. The result met clinical and parental expectations, although the cementation and excess cement removal presented a challenge owing to limited access and patient cooperation. Within these constraints, 3D-printed composite restorations demonstrated favourable clinical performance and represent a viable, minimally invasive treatment modality for managing functional and aesthetic needs in the primary dentition, particularly in cases involving dental anomalies such as ED.
Discussion
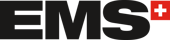
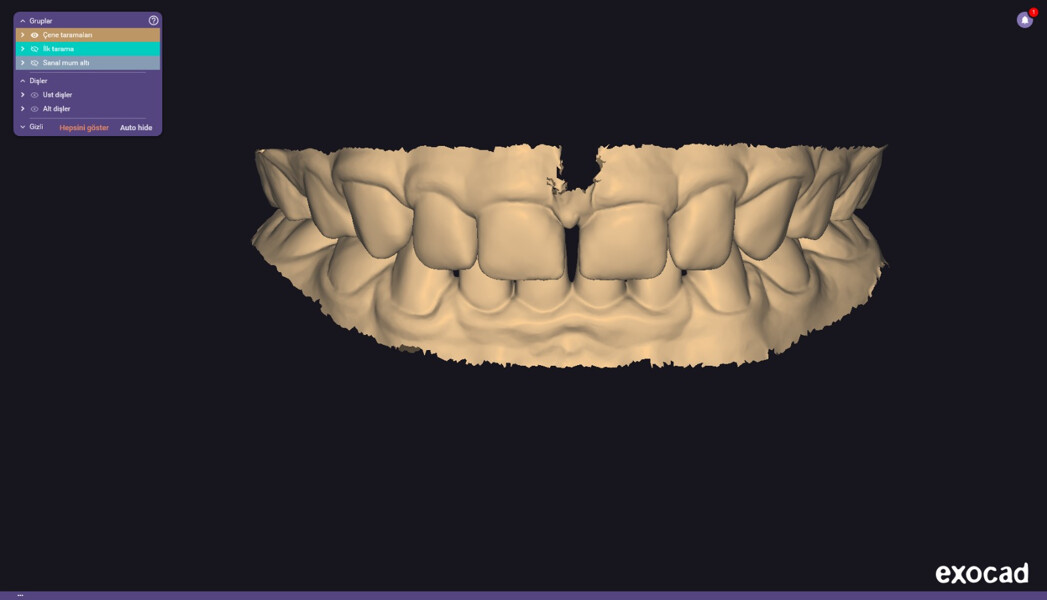
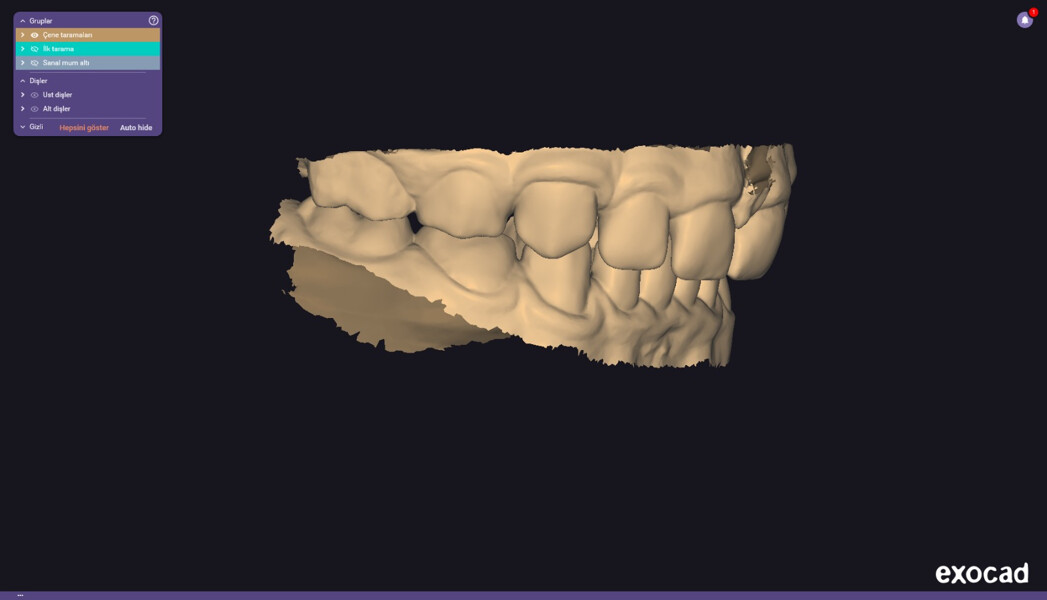
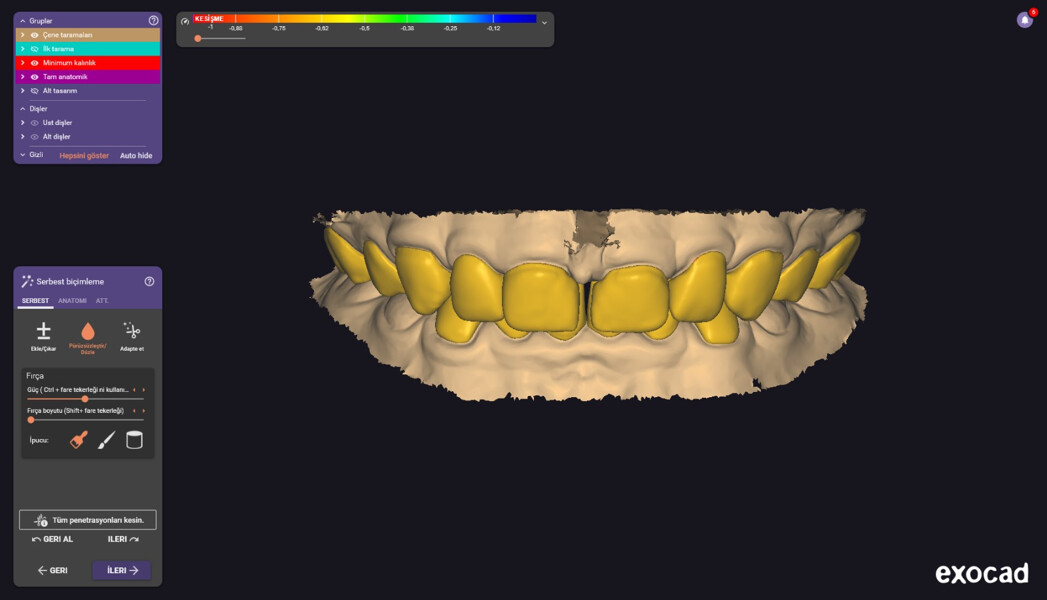
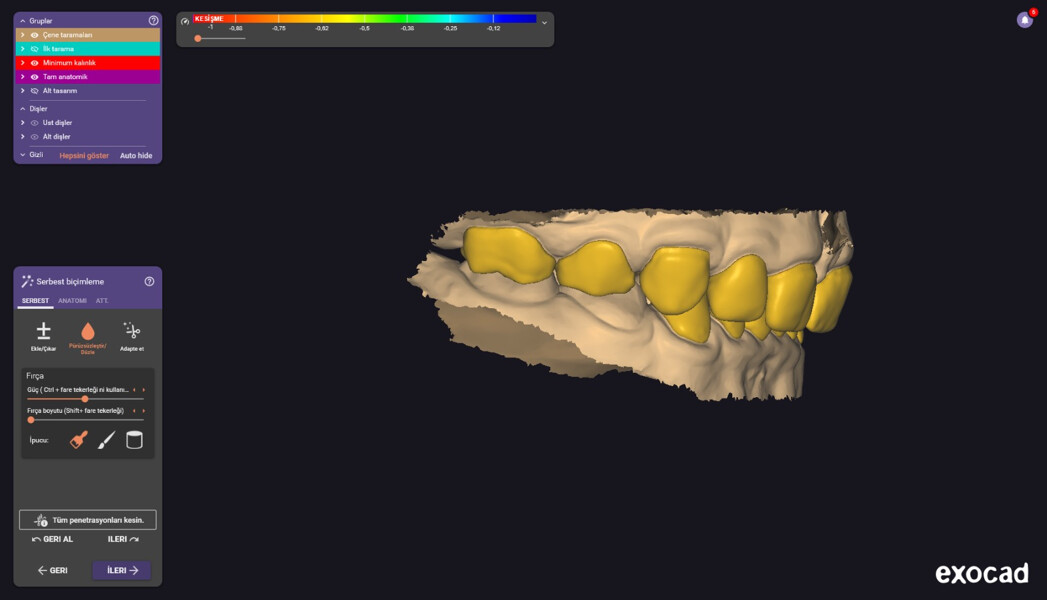
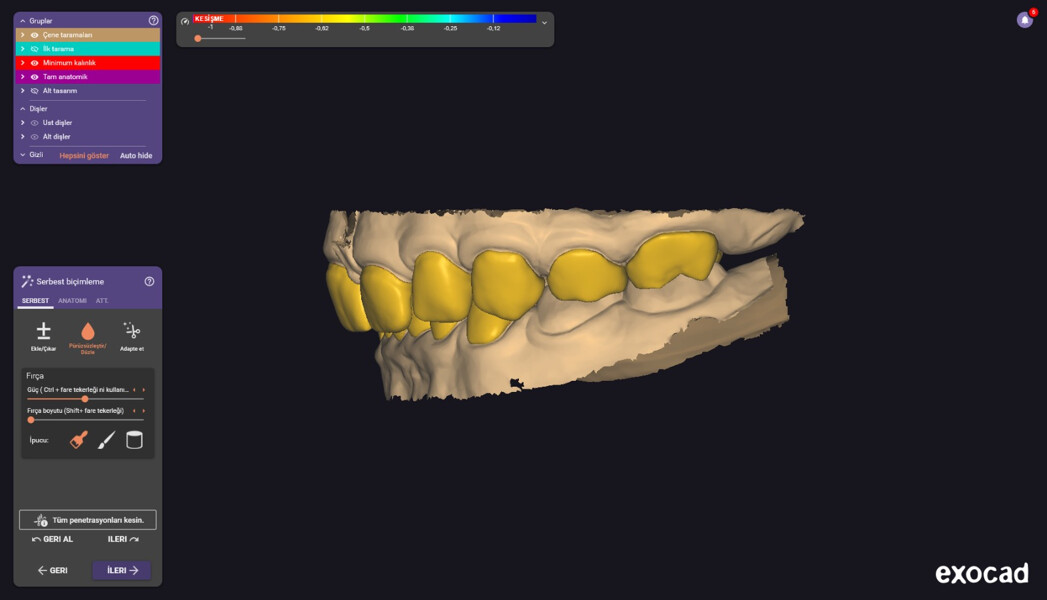
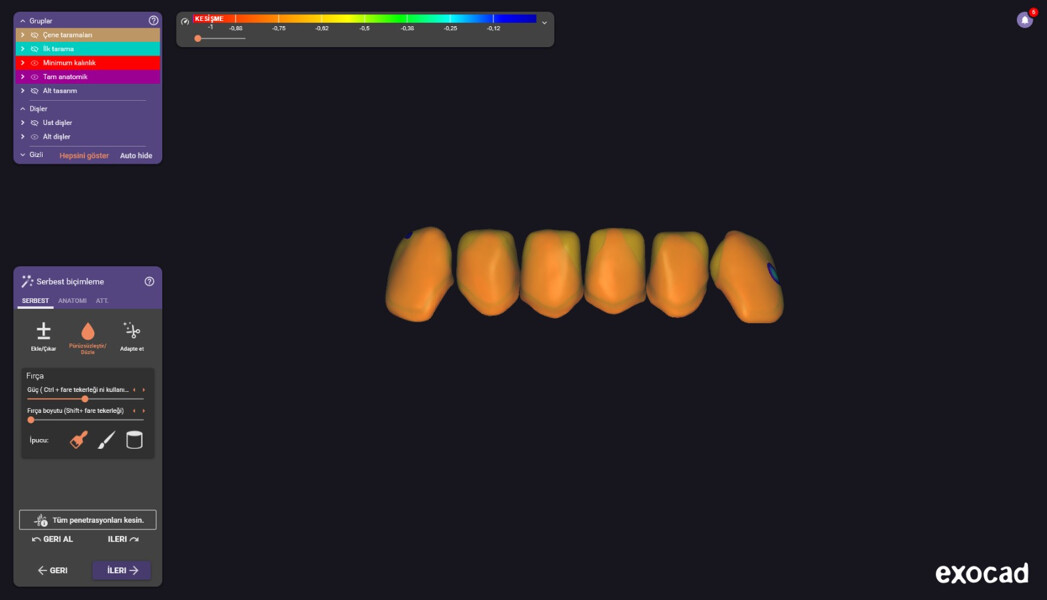
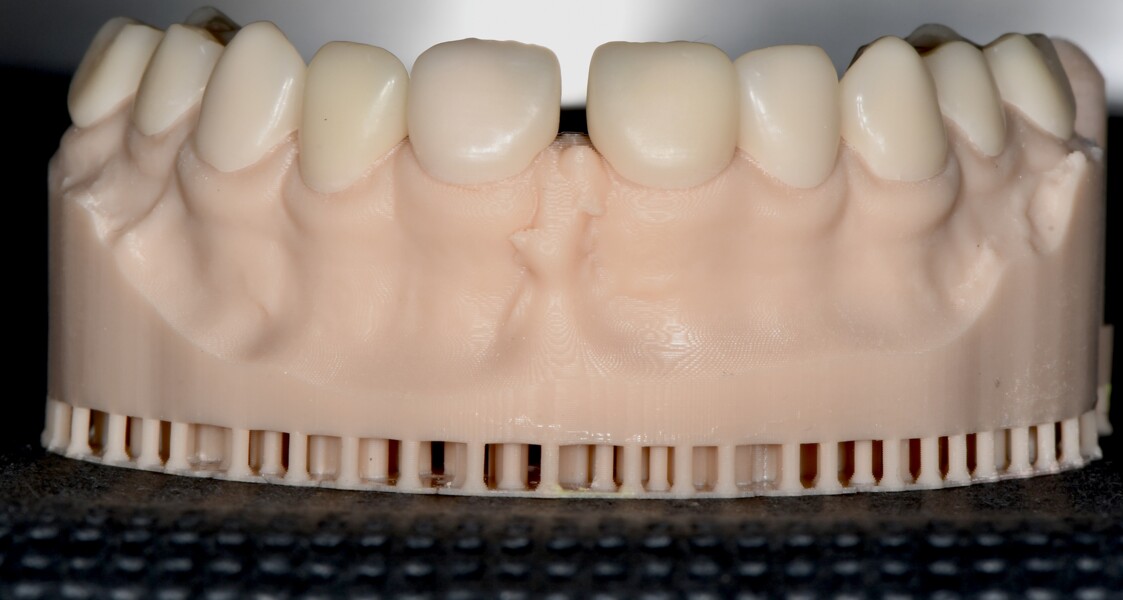
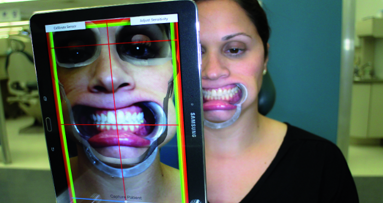
ED exhibits unique challenges in paediatric dental care owing to its early-onset impact on tooth development, facial aesthetics, oral function and psychosocial well-being. Previous studies have demonstrated that CAD/CAM-fabricated complete dentures, as well as overdentures, can be used as a solution for ED patients with a high aesthetic success rate.13 In the present case, a minimally invasive, aesthetically driven and functionally restorative approach was employed using chairside 3D-printed hybrid resin composite restorations in a 3.5-year-old child diagnosed with suspected ED. The treatment aimed to address pronounced dental anomalies, including conical anterior teeth, reduced vertical dimension of occlusion and deep overbite with mucosal impingement, all following a minimally invasive protocol owing to the patient’s age and simultaneously avoiding the use of local anaesthesia.
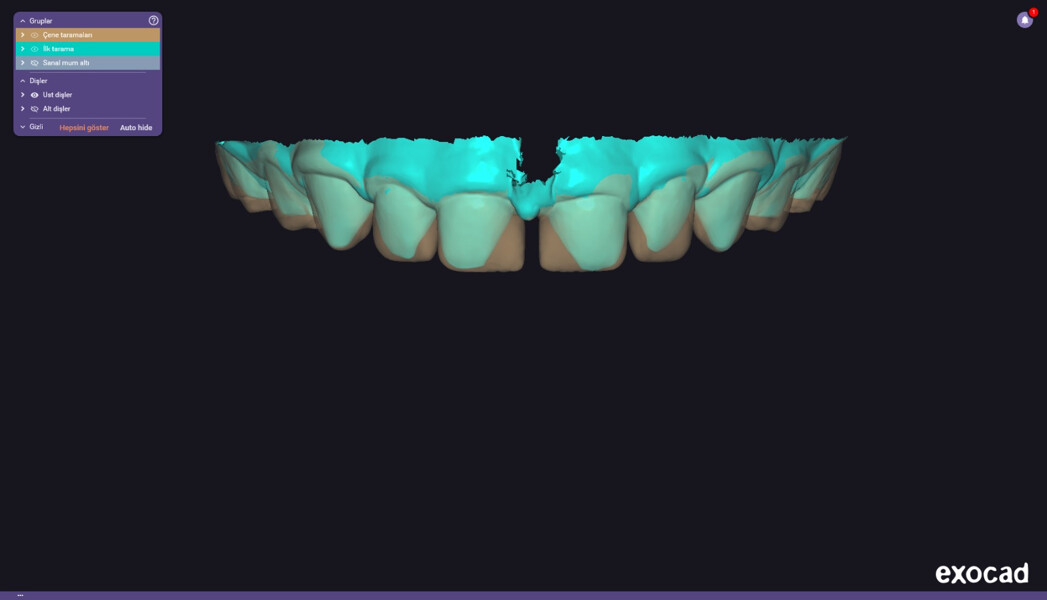
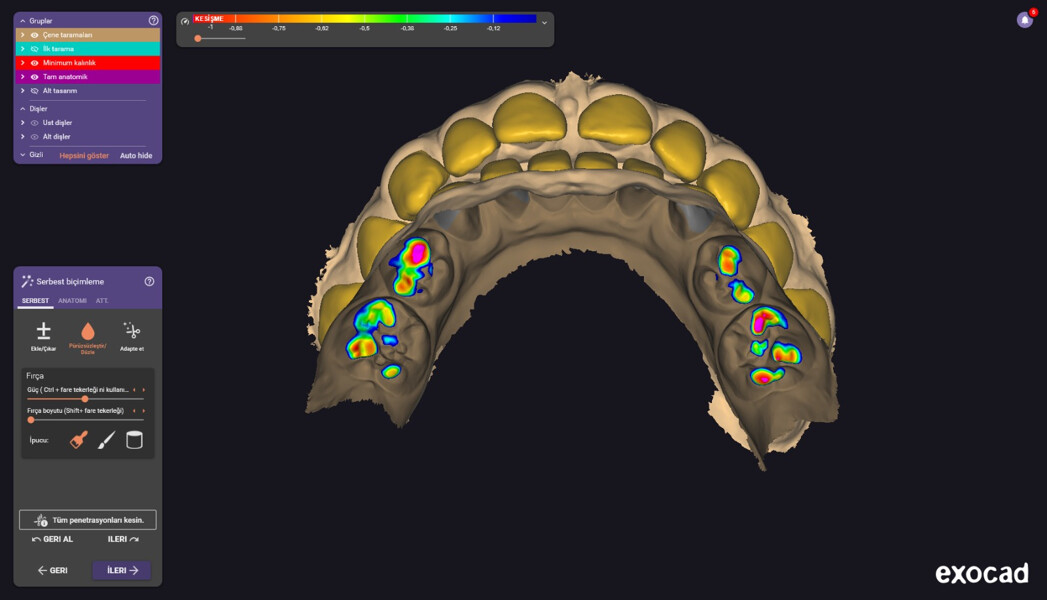
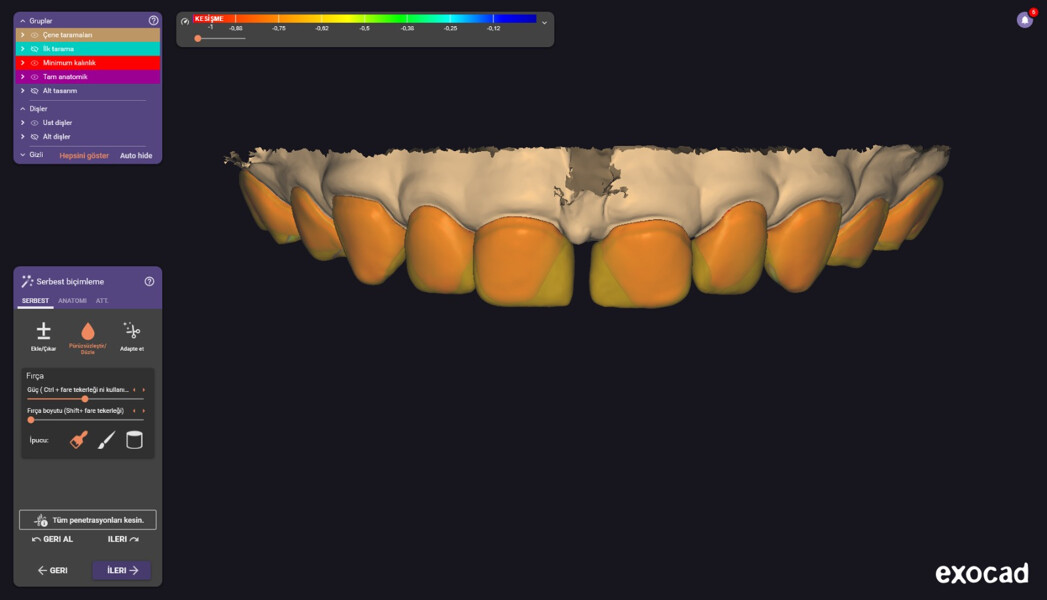
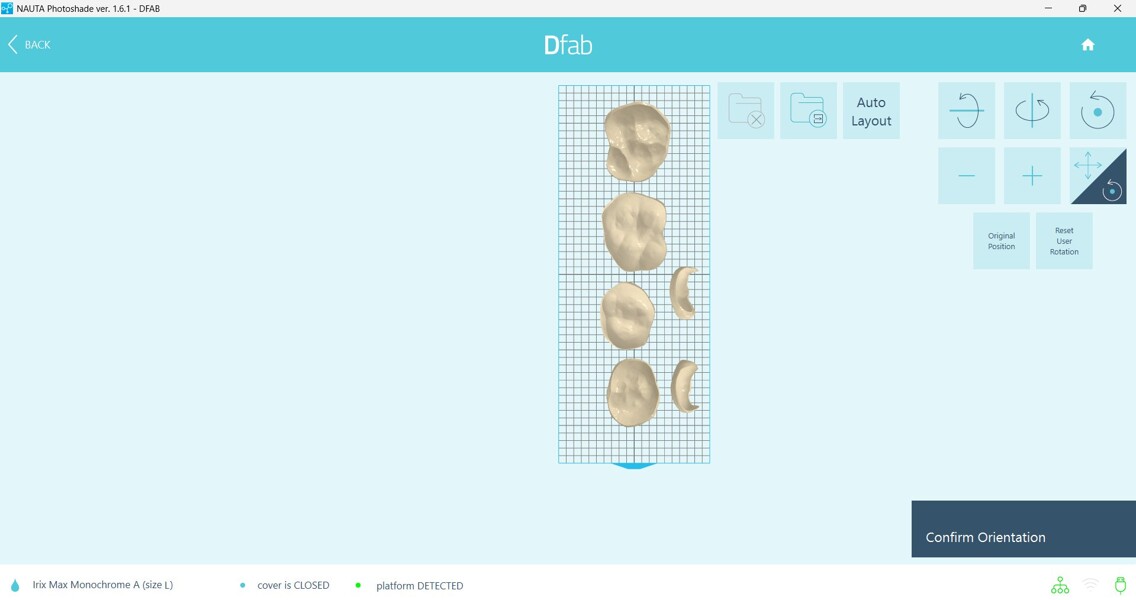
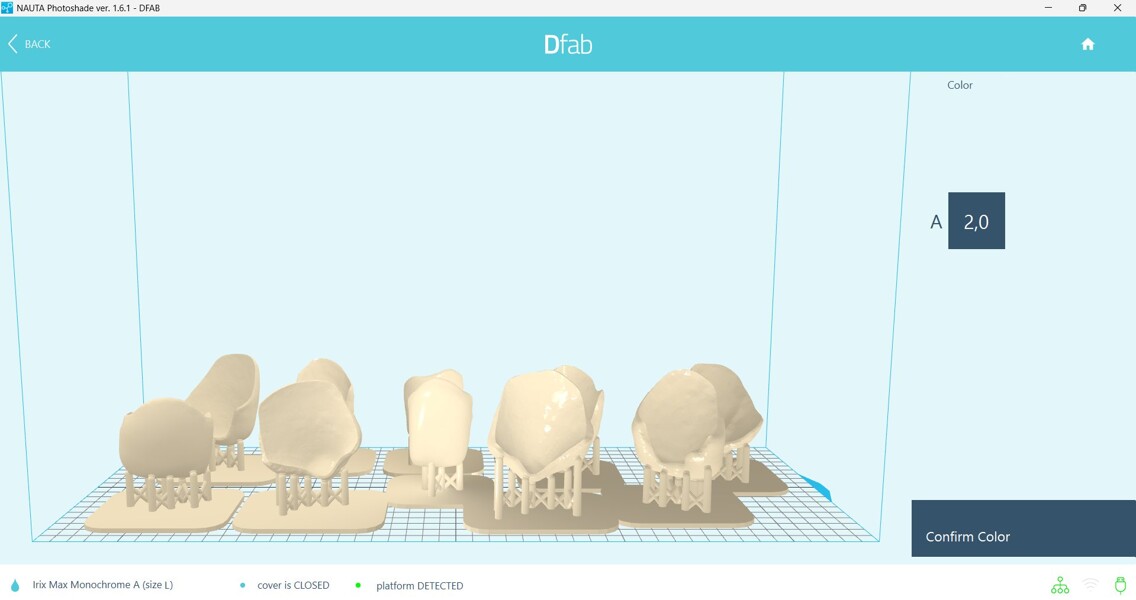
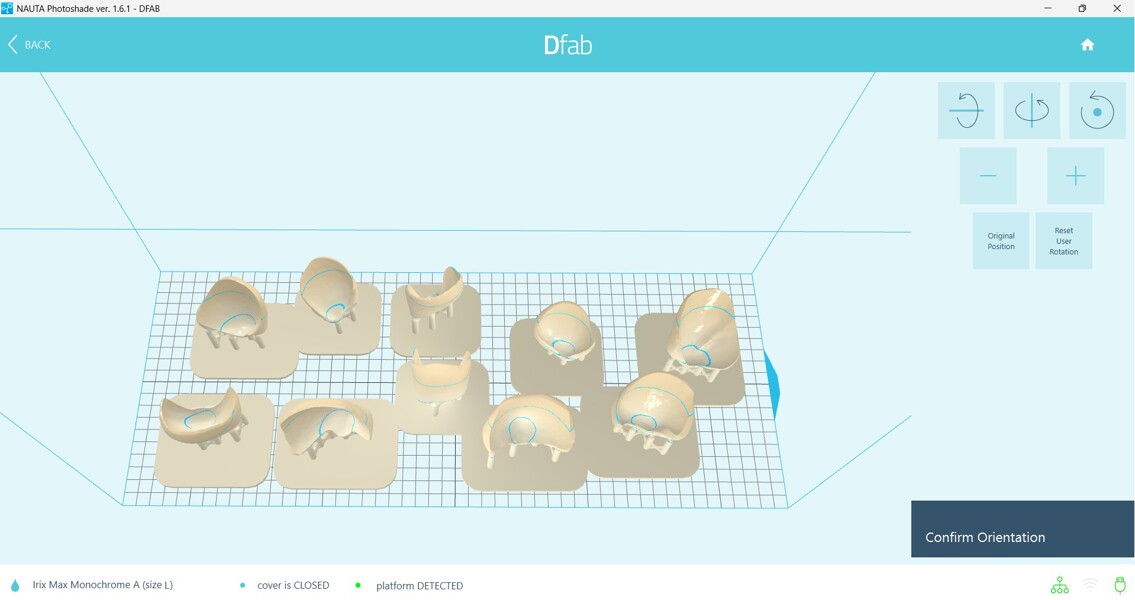
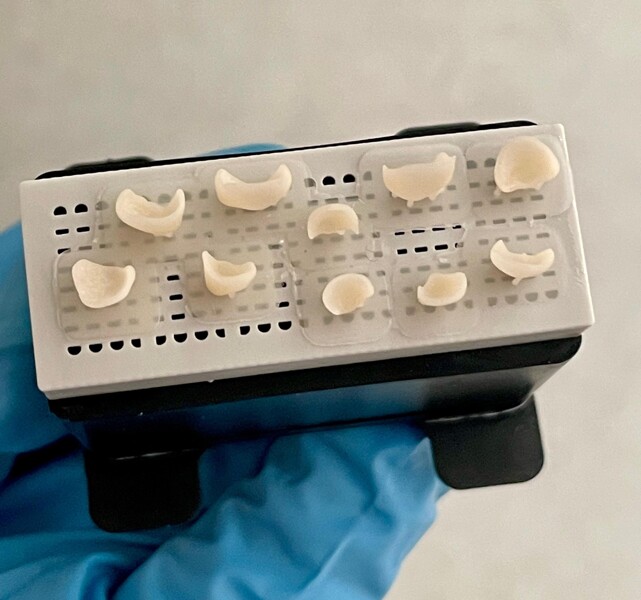
The application of the TSLA 3D-printing technology allowed for the rapid and precise fabrication of monolithic restorations tailored to the unique anatomy of a developing primary dentition. The closed-cartridge system offered significant clinical advantages, such as simplified material handling, reduced cross-contamination risk and improved workflow cleanliness, critical in paediatric settings, where treatment time and patient cooperation are limited. The use of partial restorations also facilitated relative isolation, optimised cementation conditions and enabled predictable removal of excess luting material in a paediatric setting. Previous studies have demonstrated the accuracy and clinical applicability of 3D-printed restorations using composite-based resins, supporting their use in definitive paediatric treatments.1, 6
Overall, this patient treatment supports the clinical viability of 3D-printed composite restorations as a minimally invasive, patient-centred treatment option for children with developmental dental anomalies. However, longitudinal studies are warranted to assess the long-term durability, colour stability and retention of such restorations in the primary dentition.
Conclusion
This case demonstrates the clinical feasibility and effectiveness of using 3D-printed composite restorations for minimally invasive rehabilitation of a young patient with suspected ED. The treatment achieved improvements in aesthetics, speech and function without the need for tooth preparation or local anaesthesia, key considerations in paediatric dentistry. Despite challenges related to isolation, cement removal and polishing in a very young child, the digital workflow, combined with behaviourally adapted management, enabled a predictable and well-tolerated outcome. The 3D-printed composite restorations used represent a promising option for early, patient-centred intervention in cases involving developmental dental anomalies.



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East

























































To post a reply please login or register