One proposed method to address structurally compromised teeth is crown lengthening, aimed at providing optimal conditions for tooth restoration. However, challenges arise with this approach, particularly in the aesthetic zone, where certain techniques may be limited by their impact on gingival symmetry.2, 3 The diagnostic and planning process for crown lengthening of anterior teeth is notably intricate, necessitating careful consideration to avoid potential asymmetry in gingival margins. Particularly prevalent in the aesthetic zone, notably the maxillary incisors, dentoalveolar trauma often results in the loss of coronal structure.4, 5 In such cases, restoration of the affected tooth may require additional procedures to achieve adequate supragingival height.
Surgical extrusion is a procedure through which the remaining dental structure is repositioned in a more coronal position within the alveolus.6–8 The primary objective of this technique is to elevate the affected tooth to a more coronal position, thereby creating favourable conditions for establishing an adequate ferrule, crucial for facilitating the placement of a restoration that preserves a healthy biological width.3, 7 Consequently, surgical extrusion can be a valuable approach in the treatment of severely damaged teeth, particularly in the aesthetic zone.
Surgical extrusion has various names, including intra-alveolar transplant, intentional reimplantation and forced eruption.6, 9, 10 Although the technique was initially described in 1978,11 the first case report was not published until 2002.12 Despite its early documentation, surgical extrusion remains relatively uncommon in dental practice.
Initially, the periodontal ligament is delicately loosened through syndesmotomy, followed by careful luxation facilitated by periotomes and/or elevators. Using forceps, the tooth is then gradually extruded, typically achieving a vertical displacement of 4–6 mm. To stabilise the tooth in its new position, it is immobilised for a period of two to three weeks with the aid of a flexible splint, followed by placement of a post and core and subsequently a definitive full-coverage restoration. This effective technique can be implemented with relative ease, requiring no specialised surgical expertise. Moreover, it often yields satisfactory aesthetic results, boasts a low failure rate and tends to be well received by patients.
Case series and clinical reports are classified as low-evidence literature because the causal relationships between intervention and outcomes cannot be definitively established without a control group.13, 14 Nonetheless, clinical reports can influence decision-making in dental practice,14 for example by raising awareness of new techniques, clinical approaches and research directions. The objective of this case report is to present a four-year follow-up clinical case in which a compromised anterior tooth was preserved through surgical extrusion.
Case report
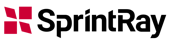
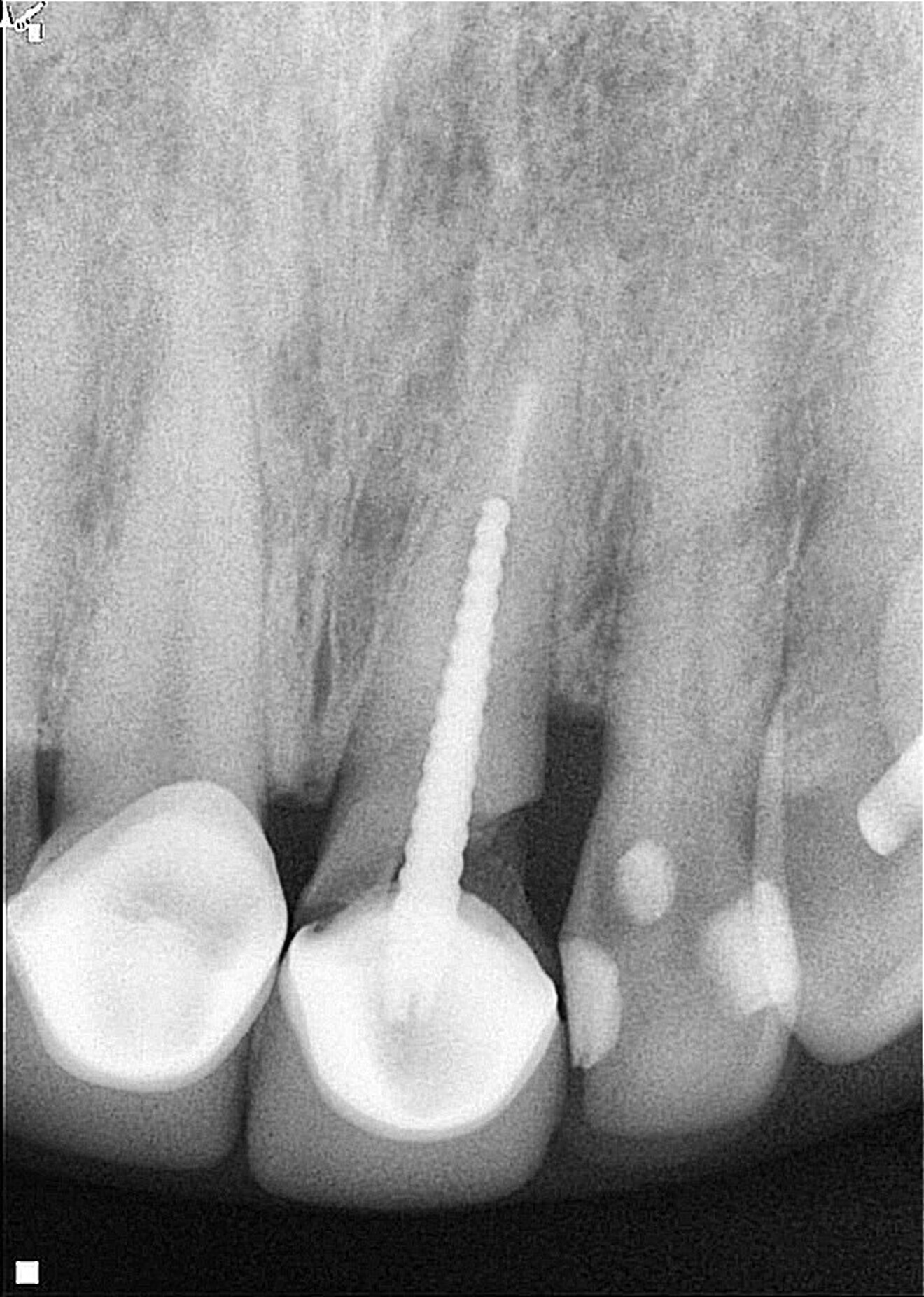
A female patient was evaluated in the dental office after a traumatic event involving her maxillary teeth. She had an oblique fracture from the mesial to distal aspect of the maxillary left central incisor at subgingival level, and the tooth’s metal post and metal–porcelain crown presented with mobility. The tooth had healthy periapical tissue (Fig. 1). Upon radiographic and clinical evaluation, it was noted that there was insufficient dental structure for a predictable restoration.15 Treatment planning included measurement and analysis of the root length, of the width of the root canal walls and of the available supragingival structure. Various treatment options were considered to save the tooth, and after a comprehensive evaluation, surgical extrusion was chosen as the preferred option to achieve adequate healthy supragingival dental structure, thereby offering the patient a favourable long-term treatment solution.6, 8



 Austria / Österreich
Austria / Österreich
 Bosnia and Herzegovina / Босна и Херцеговина
Bosnia and Herzegovina / Босна и Херцеговина
 Bulgaria / България
Bulgaria / България
 Croatia / Hrvatska
Croatia / Hrvatska
 Czech Republic & Slovakia / Česká republika & Slovensko
Czech Republic & Slovakia / Česká republika & Slovensko
 France / France
France / France
 Germany / Deutschland
Germany / Deutschland
 Greece / ΕΛΛΑΔΑ
Greece / ΕΛΛΑΔΑ
 Hungary / Hungary
Hungary / Hungary
 Italy / Italia
Italy / Italia
 Netherlands / Nederland
Netherlands / Nederland
 Nordic / Nordic
Nordic / Nordic
 Poland / Polska
Poland / Polska
 Portugal / Portugal
Portugal / Portugal
 Romania & Moldova / România & Moldova
Romania & Moldova / România & Moldova
 Slovenia / Slovenija
Slovenia / Slovenija
 Serbia & Montenegro / Србија и Црна Гора
Serbia & Montenegro / Србија и Црна Гора
 Spain / España
Spain / España
 Switzerland / Schweiz
Switzerland / Schweiz
 Turkey / Türkiye
Turkey / Türkiye
 UK & Ireland / UK & Ireland
UK & Ireland / UK & Ireland
 Brazil / Brasil
Brazil / Brasil
 Canada / Canada
Canada / Canada
 Latin America / Latinoamérica
Latin America / Latinoamérica
 USA / USA
USA / USA
 China / 中国
China / 中国
 India / भारत गणराज्य
India / भारत गणराज्य
 Pakistan / Pākistān
Pakistan / Pākistān
 Vietnam / Việt Nam
Vietnam / Việt Nam
 ASEAN / ASEAN
ASEAN / ASEAN
 Israel / מְדִינַת יִשְׂרָאֵל
Israel / מְדִינַת יִשְׂרָאֵל
 Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
Algeria, Morocco & Tunisia / الجزائر والمغرب وتونس
 Middle East / Middle East
Middle East / Middle East



















































To post a reply please login or register